Hemophilia Diagnosis: How to Spot and Confirm the Condition
When working with hemophilia diagnosis, the process of identifying a hereditary bleeding disorder by testing blood clotting ability and genetic markers. Also known as hemophilia testing, it helps doctors decide on treatment plans and family counseling. Hemophilia diagnosis is the first step toward effective care, and it ties together several related tools and concepts.
Key Tests That Make the Difference
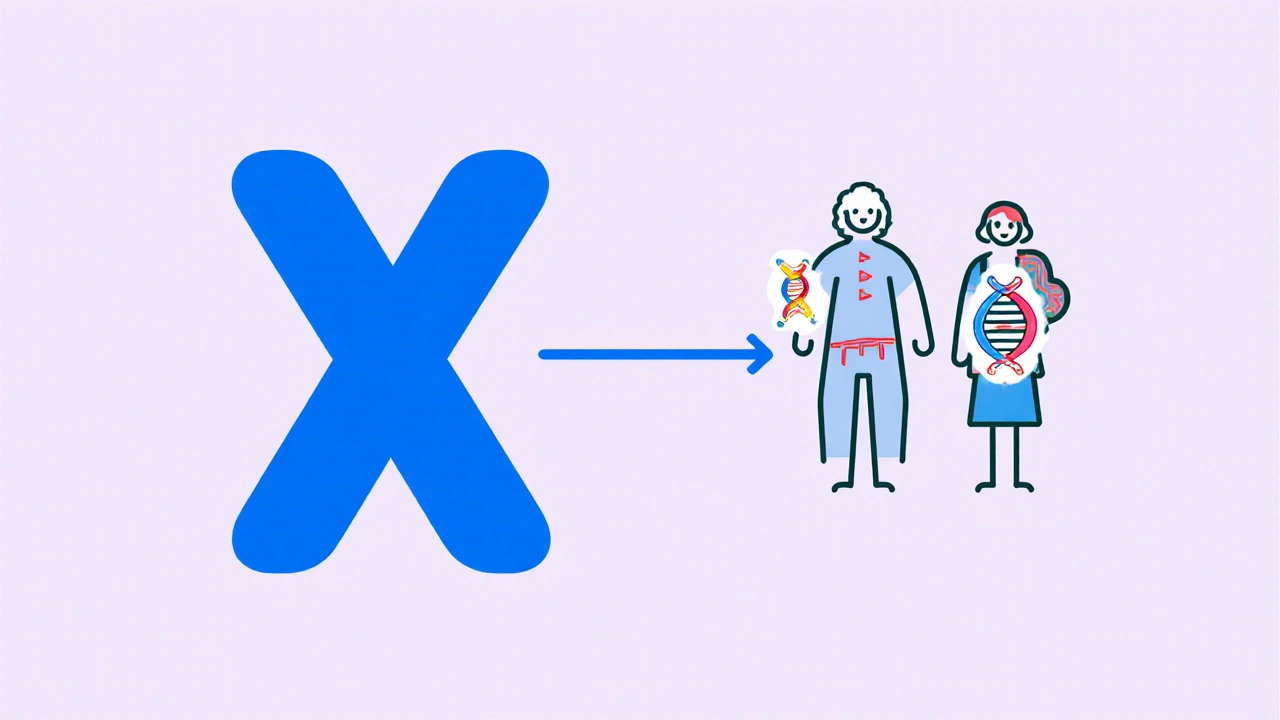
The clotting factor test, a lab analysis measuring levels of factor VIII and IX in the blood is the cornerstone of any assessment. Low levels confirm hemophilia A or B and indicate severity. This test often works hand‑in‑hand with genetic testing, DNA sequencing that spots mutations in the F8 or F9 genes. Together they form a solid diagnostic pair: the lab result tells you "what" is missing, while the genetic screen tells you "why".
Both tests fall under the broader category of a bleeding disorder, any condition where blood doesn't clot normally, leading to excessive bruising or joint bleeding. Recognizing hemophilia as part of this group helps clinicians compare it with von Willebrand disease or platelet disorders, ensuring the right follow‑up steps.
Severity grading is another crucial piece. Mild cases (factor levels >5%) often go unnoticed until surgery or trauma, while severe forms (levels <1%) cause spontaneous joint bleeds. Knowing the grade guides prophylactic therapy and informs families about bleeding risks in everyday life.
Inhibitor development adds a layer of complexity. Some patients form antibodies against replacement factors, which can render standard therapy ineffective. Testing for inhibitors early on influences whether a person will need bypass agents or novel non‑factor therapies.
For expecting parents, prenatal screening offers a head start. Chorionic villus sampling or amniocentesis can detect carrier status and fetal mutations, giving families time to plan deliveries in specialized centers. Newborn screening programs in the UK are also expanding to catch severe cases within weeks of birth.
It’s worth noting that not all clotting issues mean hemophilia. Anticoagulant medications like warfarin, a prescription drug that deliberately lowers clotting ability can mimic low factor levels in routine tests. Distinguishing drug‑induced coagulopathy from hereditary hemophilia avoids unnecessary genetic work‑ups.
Once a diagnosis is clear, treatment pathways open up. Regular factor replacement, emicizumab injections, or gene‑editing trials become options based on severity, inhibitor status, and patient preference. Early diagnosis also means early physiotherapy, which protects joints from irreversible damage.
Misdiagnosis is a real risk, especially when symptoms overlap with platelet problems or chronic joint pain from arthritis. A thorough history, repeated factor assays, and confirmatory genetic results keep errors to a minimum.
Below you’ll find a curated mix of articles that dive deeper into the tests, treatment advances, and lifestyle tips for anyone navigating hemophilia diagnosis. From lab techniques to patient stories, the collection is designed to give you practical insight and confidence as you move forward.
Hemophilia Causes, Symptoms & Diagnosis Guide
- Oct, 23 2025
- 11
Learn the genetic causes, key symptoms, and how doctors diagnose hemophilia. A concise guide for patients, families, and caregivers.
Categories
- Medication Information (114)
- Health and Wellness (52)
- Women's Health (6)
- Support Resources (5)
- Supplements (5)
- Pharmacy Reviews (5)
- Dermatology (4)
- Mental Health (4)
- Nutrition (3)
- Fitness and Wellness (3)
Archives
- March 2026 (1)
- February 2026 (12)
- January 2026 (27)
- December 2025 (30)
- November 2025 (24)
- October 2025 (29)
- September 2025 (14)
- August 2025 (2)
- July 2025 (7)
- June 2025 (2)
- May 2025 (3)
- April 2025 (4)
- online pharmacy
- dietary supplement
- medication safety
- health benefits
- side effects
- generic drugs
- drug interactions
- treatment
- wellness
- optimal health
- diabetes management
- safe medication purchase
- online pharmacy Australia
- brand name drugs
- authorized generics
- generic medications
- link
- women's health
- dietary supplements
- sleep
