Gluten-Free Diet: What It Really Means for Your Health and Medications
When you hear gluten-free diet, a dietary approach that excludes gluten, a protein found in wheat, barley, and rye. Also known as wheat-free diet, it's often recommended for people with celiac disease, a serious autoimmune condition where gluten damages the small intestine. But more people are trying it now—not just because they have a diagnosis, but because they feel better without it. The truth? Not everyone who feels better on a gluten-free diet has celiac disease. Some have non-celiac gluten sensitivity, where symptoms like bloating, fatigue, or brain fog improve when gluten is removed—even though tests come back negative.
What’s often overlooked is how a gluten-free diet, a dietary approach that excludes gluten, a protein found in wheat, barley, and rye. Also known as wheat-free diet, it's often recommended for people with celiac disease, a serious autoimmune condition where gluten damages the small intestine. can interact with your medications. Many pills, including some generics, use wheat starch as a filler. If you’re strictly avoiding gluten, even tiny amounts in your meds can cause problems. And if you’re switching to gluten-free processed foods, you might be missing key nutrients like B vitamins, iron, or fiber—things that can affect how your body absorbs drugs like levothyroxine or blood thinners. Your gut health changes when you cut out gluten, and that can change how your body handles every pill you take.
People on long-term medications—especially for thyroid, diabetes, or heart conditions—need to pay attention. A gluten-free diet, a dietary approach that excludes gluten, a protein found in wheat, barley, and rye. Also known as wheat-free diet, it's often recommended for people with celiac disease, a serious autoimmune condition where gluten damages the small intestine. isn’t a magic fix. It’s a medical tool. For some, it’s life-changing. For others, it’s unnecessary—and could even be harmful if it leads to poor nutrition or unmonitored drug interactions. That’s why the posts here cover real-world issues: how gluten-free eating affects hydration, how it can influence drug metabolism in people with liver or kidney issues, and why timing your meds matters even more when your gut is healing.
What you’ll find below aren’t just generic tips. These are practical, evidence-based insights from people managing real conditions—like how a gluten-free diet might worsen dehydration if you’re on SGLT2 inhibitors, or how switching to gluten-free meds without checking ingredients can trigger symptoms in someone with celiac disease. This isn’t about trends. It’s about safety, clarity, and what actually works when your health depends on both what you eat and what you take.
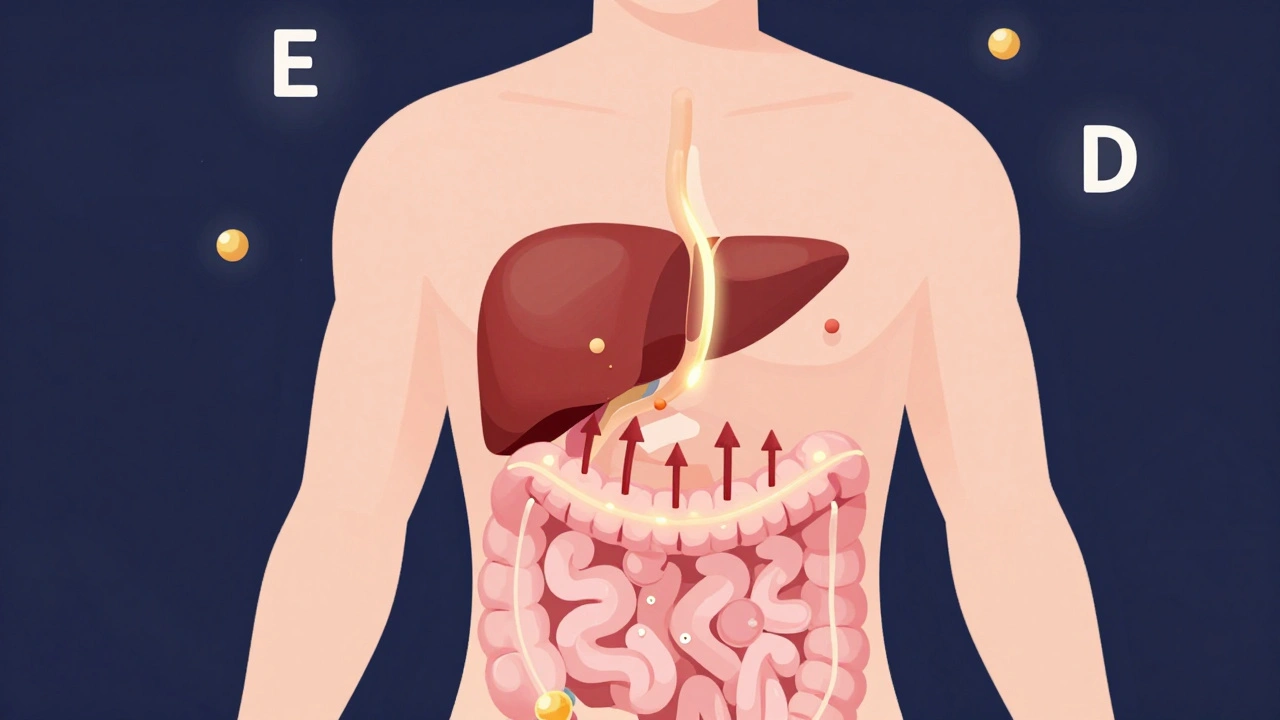
Celiac Disease and Liver Abnormalities: What Links Them
- Dec, 5 2025
- 10
Celiac disease can cause liver enzyme elevations and fatty liver in up to 40% of untreated cases. The good news? Most liver abnormalities reverse with a strict gluten-free diet - but only if you eat whole foods, not processed gluten-free junk.
Categories
- Medication Information (113)
- Health and Wellness (52)
- Women's Health (6)
- Support Resources (5)
- Supplements (5)
- Pharmacy Reviews (5)
- Dermatology (4)
- Mental Health (4)
- Nutrition (3)
- Fitness and Wellness (3)
Archives
- February 2026 (12)
- January 2026 (27)
- December 2025 (30)
- November 2025 (24)
- October 2025 (29)
- September 2025 (14)
- August 2025 (2)
- July 2025 (7)
- June 2025 (2)
- May 2025 (3)
- April 2025 (4)
- March 2025 (3)
- online pharmacy
- dietary supplement
- medication safety
- health benefits
- side effects
- generic drugs
- drug interactions
- treatment
- wellness
- optimal health
- diabetes management
- safe medication purchase
- online pharmacy Australia
- brand name drugs
- authorized generics
- generic medications
- link
- women's health
- dietary supplements
- sleep
