Estrogen Replacement: What It Is, Who Needs It, and What You Should Know
When your body starts making less estrogen, a key female hormone that regulates the menstrual cycle, supports bone density, and influences mood and skin health. Also known as hormone replacement therapy, it’s often used to ease the transition through menopause and prevent long-term health risks tied to low hormone levels. Estrogen isn’t just about hot flashes—it plays a role in your brain, heart, bladder, and even your bones. When levels drop, things like night sweats, vaginal dryness, mood swings, and even bone thinning can start showing up. For many women, estrogen replacement isn’t optional—it’s a way to take back control.
But not everyone needs it, and not all forms work the same. hormone therapy, a broad term covering estrogen alone or combined with progesterone. Also known as menopausal hormone therapy, it’s tailored based on whether you’ve had a hysterectomy, your age, and your personal health history. If you’ve had your uterus removed, you can take estrogen by itself. If you still have it, you’ll need progesterone too, or you risk uterine cancer. The delivery method matters too—pills, patches, gels, or vaginal rings all have different pros and cons. Some women prefer patches to avoid liver stress. Others choose creams for targeted relief without full-body exposure.
Estrogen replacement doesn’t exist in a vacuum. It connects to other treatments you might be using. For example, if you’re taking calcium and iron supplements, commonly used to protect bone health and prevent anemia during and after menopause, timing matters. These can block estrogen absorption if taken at the same time. Same goes for thyroid meds or certain antibiotics. Your doctor needs to know everything you’re on. And while estrogen helps with bone density, it’s not a replacement for weight-bearing exercise or vitamin D. It’s one tool in a bigger toolkit.
Some women worry about risks—breast cancer, blood clots, stroke. The truth? For most healthy women under 60, the benefits outweigh the risks, especially if started close to menopause. But if you’ve had a blood clot, certain cancers, or liver disease, estrogen isn’t for you. That’s why personalized advice matters. It’s not one-size-fits-all. Your age, family history, symptoms, and lifestyle all shape the decision.
Below, you’ll find real, practical guides that dig into the details: how estrogen interacts with other meds, what alternatives exist, and how to manage side effects without giving up your quality of life. These aren’t theoretical—they’re written for women who want to understand what’s happening in their bodies and make smart, informed choices.
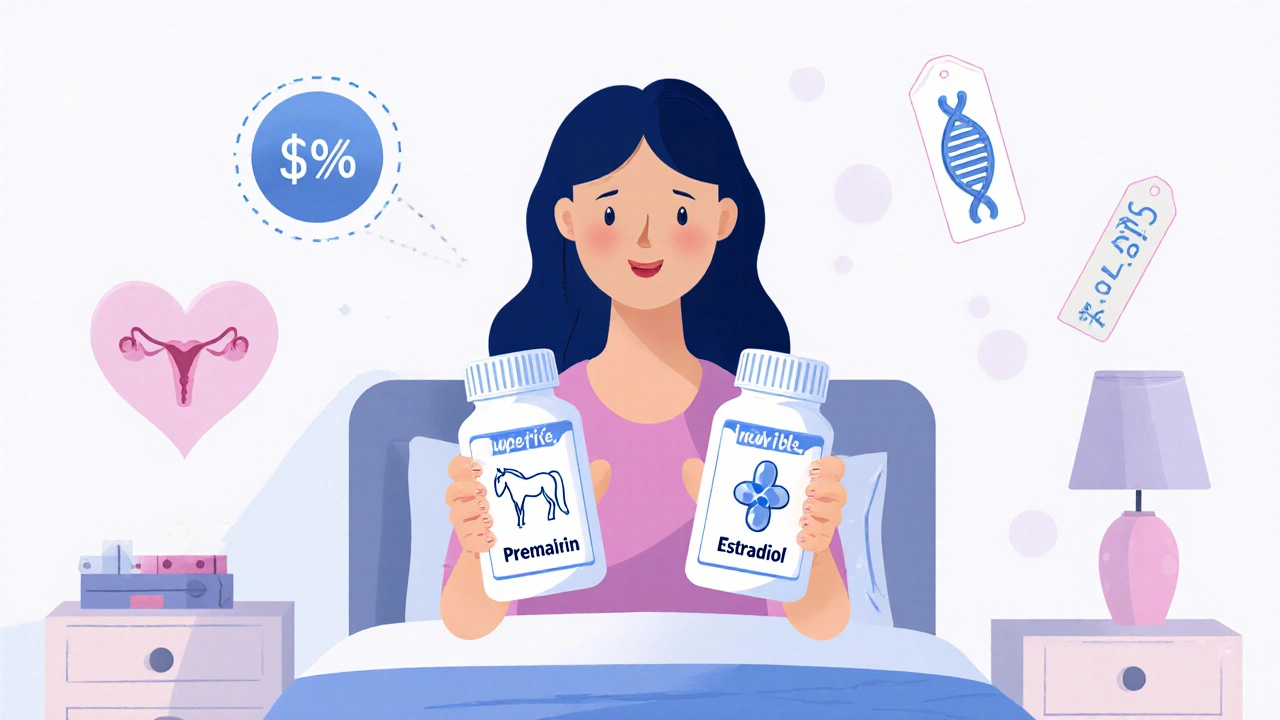
Compare Premarin (Conjugated Estrogens) with Alternatives: What Works Best in 2025
- Oct, 28 2025
- 14
Compare Premarin with safer, more affordable alternatives like estradiol, vaginal estrogen, and non-hormonal options for menopause symptoms in 2025. Learn what works best and how to choose.
Categories
- Medication Information (111)
- Health and Wellness (52)
- Women's Health (6)
- Support Resources (5)
- Supplements (5)
- Pharmacy Reviews (5)
- Dermatology (4)
- Mental Health (4)
- Nutrition (3)
- Fitness and Wellness (3)
Archives
- February 2026 (10)
- January 2026 (27)
- December 2025 (30)
- November 2025 (24)
- October 2025 (29)
- September 2025 (14)
- August 2025 (2)
- July 2025 (7)
- June 2025 (2)
- May 2025 (3)
- April 2025 (4)
- March 2025 (3)
- online pharmacy
- dietary supplement
- medication safety
- health benefits
- side effects
- generic drugs
- treatment
- wellness
- optimal health
- diabetes management
- safe medication purchase
- online pharmacy Australia
- brand name drugs
- drug interactions
- authorized generics
- generic medications
- link
- women's health
- dietary supplements
- sleep
