Compare Premarin (Conjugated Estrogens) with Alternatives: What Works Best in 2025
 Oct, 28 2025
Oct, 28 2025
Menopause Treatment Decision Calculator
Find Your Best Menopause Treatment
This tool helps you identify the most appropriate treatment option based on your symptoms and medical history. Always consult your doctor before starting or changing any treatment.
Important: This tool provides general guidance based on current medical knowledge. Your specific situation requires personalized medical advice from your healthcare provider.
Always discuss treatment options with your doctor to determine the safest and most effective approach for your individual needs.
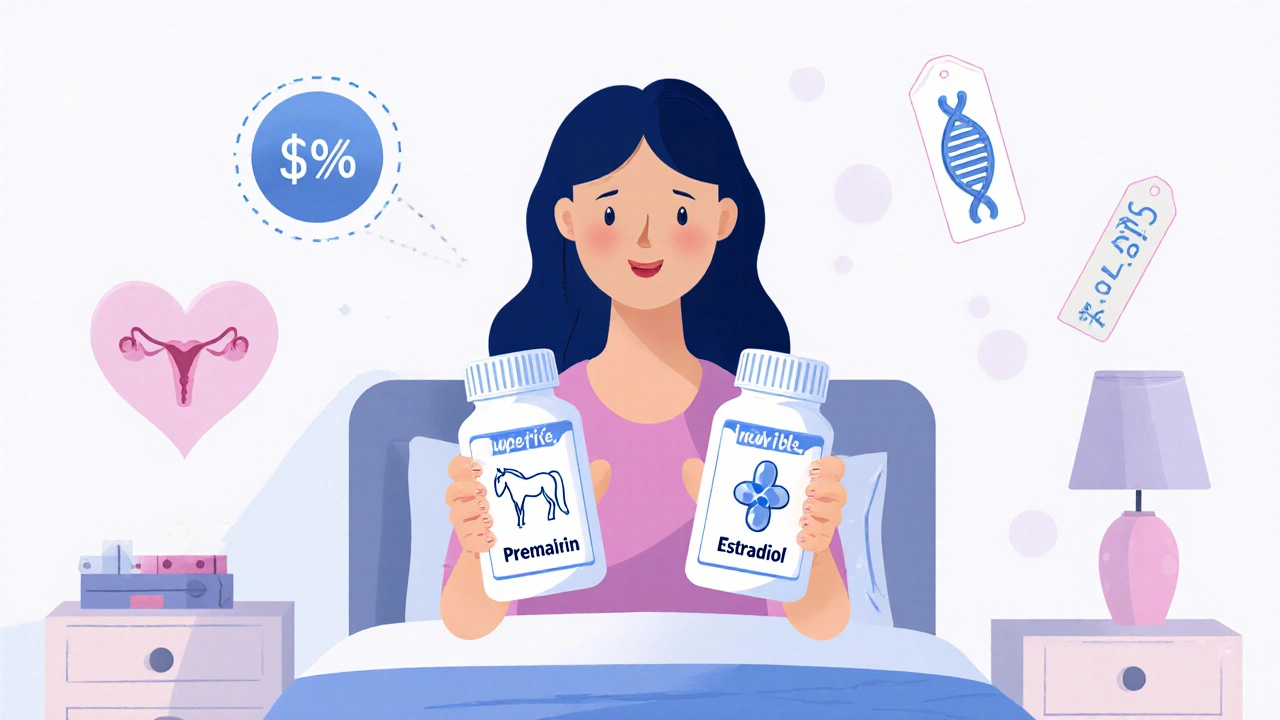
When women start experiencing menopause symptoms like hot flashes, night sweats, vaginal dryness, or mood swings, doctors often talk about hormone therapy. One of the oldest and most prescribed options has been Premarin - a brand name for conjugated estrogens derived from pregnant mare urine. But in 2025, many women and their doctors are asking: are there better, safer, or more natural options out there?
Premarin has been on the market since the 1940s. It works. It reduces symptoms. But it’s not the only choice anymore. And with newer research, growing concerns about long-term risks, and a wider range of alternatives, it’s time to compare what’s available - not just in terms of effectiveness, but safety, cost, and personal fit.
What is Premarin, and how does it work?
Premarin contains a mix of 10 different estrogens, all extracted from the urine of pregnant horses. That’s where the name comes from - PREgnant MARes’ IN urine. These estrogens, including estrone sulfate and equilin sulfate, mimic human estrogen and help balance hormone levels during menopause.
It’s taken as a pill, usually once daily. Doctors often prescribe it for women with moderate to severe menopausal symptoms who aren’t candidates for non-hormonal treatments. It’s also used for preventing osteoporosis in postmenopausal women at high risk.
But here’s the catch: because Premarin contains horse-derived estrogens, they’re not identical to the estrogens your body naturally makes. That mismatch may contribute to side effects like bloating, breast tenderness, and - more seriously - a higher risk of blood clots, stroke, and breast cancer when used long-term, especially when combined with progestin.
Why look for alternatives to Premarin?
Since the 2002 Women’s Health Initiative study, doctors have become much more cautious about prescribing hormone therapy. That landmark trial showed that long-term use of Premarin plus progestin increased the risk of heart disease, stroke, blood clots, and breast cancer in women over 50.
Today, guidelines from the North American Menopause Society and the Endocrine Society recommend hormone therapy only for women with moderate to severe symptoms, at the lowest effective dose, and for the shortest time possible.
Many women now want options that feel more natural, have fewer side effects, or are easier to tolerate. Others are concerned about animal-derived ingredients or ethical sourcing. Some are simply looking for something cheaper - Premarin can cost over $100 a month without insurance.
Bioidentical Estrogen: Estradiol as the Top Alternative
The most common and clinically supported alternative to Premarin is estradiol. Unlike Premarin, estradiol is chemically identical to the primary estrogen your body produces before menopause. It’s available as pills, patches, gels, sprays, and vaginal rings.
Brands like EstroGel, Activella, and generic estradiol tablets are widely used. Studies show estradiol is just as effective as Premarin for relieving hot flashes and vaginal atrophy - but with a lower risk profile.
A 2023 analysis in The Journal of Clinical Endocrinology & Metabolism found that transdermal estradiol (patches or gels) reduced the risk of blood clots by 40% compared to oral conjugated estrogens like Premarin. That’s because it bypasses the liver, avoiding the first-pass metabolism that can increase clotting factors.
Many women prefer estradiol because:
- It’s human-identical, not horse-derived
- Lower risk of blood clots, especially with patches
- More predictable dosing
- Available in generic form for as low as $10-$15/month
Vaginal Estrogen: For Local Symptoms Only
If your main issue is vaginal dryness, itching, or painful sex - not hot flashes - you don’t need systemic hormones. Vaginal estrogen products like Imvexxy, Vagifem, or Estring deliver low doses directly to the tissue.
These are often overlooked, but they’re highly effective for urinary and vaginal symptoms. Because very little estrogen enters the bloodstream, the risks are minimal. You can use them long-term without the same concerns as oral therapy.
For women who’ve had breast cancer or are at high risk, non-hormonal vaginal moisturizers like Replens or lubricants like Hyalo Gyn can help - though they don’t reverse tissue thinning like estrogen does.
Non-Hormonal Options: What Actually Works?
Not everyone wants hormones. That’s okay. There are FDA-approved non-hormonal treatments for hot flashes and night sweats.
Fezolinetant (brand name Veozah) is the newest. Approved in 2023, it works by blocking a brain receptor (NK3) that triggers hot flashes. In trials, it reduced hot flashes by 50-70%. Side effects include mild diarrhea and elevated liver enzymes - so liver function needs monitoring.
Paroxetine (Brisdelle) is the only non-hormonal antidepressant approved specifically for hot flashes. It’s a low-dose SSRI. Works for about 60% of users. Can cause nausea, fatigue, or weight gain.
Other options like gabapentin, clonidine, or lifestyle changes (cooling techniques, weight loss, avoiding alcohol/spicy foods) help some women - but not as reliably as hormones.
Plant-Based and Herbal Alternatives: Do They Work?
Black cohosh, red clover, soy isoflavones, and evening primrose oil are popular. But here’s the truth: most studies show they work no better than a placebo for hot flashes. The National Institutes of Health reviewed over 50 trials and found no consistent benefit.
Some women swear by them. But there’s little regulation. A 2024 Consumer Reports test of 12 black cohosh supplements found that 3 had no active ingredient at all. Others contained contaminants.
Herbal options aren’t risk-free either. Black cohosh has been linked to rare liver damage. Soy can interfere with thyroid meds. Don’t assume “natural” means safe.
Cost Comparison: What’s Affordable in 2025?
Cost matters. Here’s a rough estimate for a 30-day supply, based on U.S. pharmacy prices (without insurance):
| Medication | Form | Approx. Cost (USD) | Generic Available? | Insurance Coverage |
|---|---|---|---|---|
| Premarin | Oral tablet | $110-$150 | No | Often requires prior authorization |
| Estradiol | Oral tablet | $10-$20 | Yes | Widely covered |
| Estradiol | Transdermal gel | $80-$120 | Yes (limited) | Usually covered |
| Fezolinetant (Veozah) | Oral tablet | $400-$500 | No | Requires step therapy |
| Vagifem | Vaginal tablet | $100-$130 | Yes | Often covered |
Generic estradiol is the clear winner for affordability and effectiveness. If you’re paying over $50 a month for estrogen therapy, you’re likely overpaying.
Who Should Avoid Premarin and Alternatives?
Not everyone is a candidate for estrogen therapy. You should avoid all forms of estrogen if you have:
- History of breast cancer
- History of blood clots, stroke, or heart attack
- Unexplained vaginal bleeding
- Active liver disease
- Pregnancy
Women with a history of migraines with aura, severe hypertension, or certain genetic clotting disorders also need to be cautious. Always get tested for risk factors before starting any hormone therapy.
How to Choose the Right Option for You
There’s no one-size-fits-all. Here’s how to decide:
- What are your main symptoms? Hot flashes? Vaginal dryness? Both?
- What’s your risk for blood clots or breast cancer? (Ask your doctor about family history, BMI, smoking status)
- Do you prefer pills, patches, or gels? (Patches avoid liver stress)
- Can you afford it? Generic estradiol is the most cost-effective.
- Are you comfortable with animal-derived ingredients? (If not, avoid Premarin)
If you’re under 60 and within 10 years of menopause onset, hormone therapy is generally safe for symptom relief. The benefits often outweigh the risks. But if you’re over 65, or have multiple risk factors, non-hormonal options are safer.
What’s Next After Stopping Premarin?
If you’ve been on Premarin for years and want to stop, don’t quit cold turkey. Withdrawal can trigger severe rebound hot flashes. Work with your doctor to taper slowly - maybe reduce by 0.3 mg every 2-4 weeks.
Switching to estradiol? You can often switch directly, but your dose may need adjustment. A 0.625 mg Premarin tablet is roughly equivalent to 1 mg estradiol - but everyone’s body responds differently. Your doctor will monitor symptoms and blood levels if needed.
Many women find that after switching from Premarin to estradiol, their bloating and breast tenderness improve within weeks. Some report better sleep and mood stability too.
Final Thoughts: Premarin Is Not the Only Choice
Premarin saved lives and eased suffering for generations. But medicine has moved on. In 2025, we have safer, more targeted, and more affordable options. Estradiol - especially in transdermal form - is the new standard of care for most women needing systemic estrogen therapy.
Don’t feel stuck with what your doctor prescribed years ago. Ask for alternatives. Ask about generics. Ask about non-hormonal options. Your body, your choices.
If your symptoms are mild, try lifestyle changes first. If they’re severe, don’t suffer in silence - there are real solutions that work without the risks of old-school hormone therapy.
Is Premarin still prescribed today?
Yes, but less often than before. Doctors still prescribe Premarin for women who don’t respond to estradiol or have specific insurance restrictions. However, most new prescriptions now favor generic estradiol due to better safety data and lower cost.
Can I switch from Premarin to estradiol on my own?
No. Never switch hormone medications without medical supervision. Dosing isn’t always direct, and stopping suddenly can cause severe withdrawal symptoms. Your doctor will help you taper off Premarin and start estradiol safely, adjusting the dose based on your symptoms and blood work if needed.
Are bioidentical hormones safer than Premarin?
Bioidentical estradiol (like generic estradiol pills or patches) is safer than Premarin because it matches human estrogen exactly and has lower clotting risks. But compounded bioidentical hormones - made in specialty pharmacies - are not FDA-regulated. Their strength, purity, and safety aren’t guaranteed. Stick to FDA-approved estradiol products.
Does estrogen therapy cause weight gain?
Estrogen therapy doesn’t directly cause weight gain. But menopause itself slows metabolism and shifts fat to the abdomen. Some women feel bloated on estrogen, which can feel like weight gain. In fact, estrogen can help preserve muscle mass and improve insulin sensitivity, which may help manage weight.
How long can I safely take estrogen therapy?
For most women under 60 and within 10 years of menopause, short-term use (up to 5-7 years) is considered safe for symptom relief. Long-term use beyond 10 years increases risks. The goal is to use the lowest dose for the shortest time needed. Reassess every year with your doctor.
What if I can’t afford estradiol?
Generic estradiol is often under $15 a month at pharmacies like Walmart, Costco, or through GoodRx coupons. If you’re still struggling, ask your doctor about patient assistance programs. Some manufacturers offer free or discounted medication for low-income patients. Non-hormonal options like Veozah or paroxetine may be covered by insurance even if estrogen isn’t.

krishna raut
October 28, 2025 AT 18:59Generic estradiol is the way to go. $15/month vs $150? No contest. I switched last year and my bloating vanished.
Prakash pawar
October 28, 2025 AT 19:23Look man we’ve been brainwashed by Big Pharma to think hormones are the only answer but nature gave us plants for a reason why do we keep ignoring the wisdom of our ancestors
MOLLY SURNO
October 30, 2025 AT 13:43This is one of the most balanced and well-researched summaries I’ve read on menopause therapy. Thank you for clearly outlining the risks, benefits, and alternatives. It’s refreshing to see evidence-based information presented without sensationalism.
Alex Hundert
October 30, 2025 AT 14:38Stop letting insurance companies dictate your treatment. If your doctor still pushes Premarin, find a new doctor. Estradiol patches are safer, cheaper, and more effective. This isn’t debate material-it’s medical fact.
Emily Kidd
October 30, 2025 AT 19:15veozah is wild but like… i tried it and my hot flashes dropped by like 80% but i got the runs for a week 😅 worth it? kinda. also generic estradiol is a godsend
Justin Cheah
November 1, 2025 AT 13:10Let’s be real-Premarin was never about women’s health. It was a cash cow for Pfizer and horse farms. The WHI study was buried for years. Now they’re pushing Veozah at $500/month because they need a new monopoly. Bioidentical? FDA-approved estradiol is the only real option. Everything else is a distraction funded by supplement marketers. And don’t get me started on black cohosh-half those pills are just sawdust with a label. You’re paying for placebo and a dream.
caiden gilbert
November 2, 2025 AT 03:13Switching from Premarin to estradiol felt like trading a rusty bicycle for a Tesla. No more foggy brain, no more bloating like I’d swallowed a beach ball. And the best part? I can finally wear white pants again without feeling like I’m auditioning for a soap opera.
phenter mine
November 3, 2025 AT 17:22just switched to estradiol gel last month and wow it’s been a game changer. my skin feels better too. i think i spelled gel wrong but you know what i mean 😅
Aditya Singh
November 5, 2025 AT 13:06While the pharmacokinetic profile of transdermal estradiol demonstrably reduces hepatic first-pass metabolism, thereby attenuating the upregulation of coagulation factors II, VII, IX, and X, it’s critical to contextualize this within the broader paradigm of estrogen receptor subtype selectivity. Premarin’s equine-derived estrogens exhibit differential binding affinities to ERα and ERβ, which may explain the higher incidence of thromboembolic events. Yet, the literature remains confounded by cohort heterogeneity and confounding variables such as BMI and smoking status. Thus, the assertion that estradiol is universally superior lacks robust meta-analytical validation.
Katherine Reinarz
November 5, 2025 AT 17:54i just got off premarin and now i’m crying because my husband says i’m ‘less emotional’ and i miss the drama 😭 also my vagina feels like sandpaper now help
John Kane
November 6, 2025 AT 19:32Hey everyone-whether you’re on Premarin, estradiol, Veozah, or just trying yoga and cold showers, you’re doing the hard work of taking care of yourself. Menopause isn’t a disease to be cured-it’s a life transition, and you’re navigating it with courage. Don’t let anyone make you feel like you’re not doing it right. Some of us need hormones. Some of us need herbs. Some of us need a good cry and a cup of tea. All of it counts. You’re not alone in this. And if you’re reading this, you’re already ahead of the game. Keep asking questions. Keep advocating. You’ve got this 💪🌸
Callum Breden
November 6, 2025 AT 23:37The entire premise of this article is dangerously misleading. To suggest that estradiol is ‘safer’ than conjugated estrogens is to ignore the absence of long-term, randomized, placebo-controlled trials demonstrating reduced cardiovascular mortality. The WHI data remains the gold standard. Furthermore, the promotion of generic estradiol as a panacea reflects the corrosive influence of pharmaceutical cost-cutting culture. This is not medicine-it is commodification of menopause.
Mansi Gupta
November 7, 2025 AT 03:32I appreciate the thorough breakdown. I’ve been on estradiol patches for two years and have felt much more like myself. I was hesitant at first, but after discussing risks with my doctor and getting blood work done, it was the right choice. Thank you for highlighting that non-hormonal options exist too-it helps people feel less pressured to choose hormones.
Erin Corcoran
November 8, 2025 AT 02:14just wanna say that vaginal estrogen changed my life 🥹 i was so embarrassed to talk about it but now i can actually wear leggings again 😭 also if you’re scared of hormones-veozah is a legit alternative, even if it’s pricey. my insurance covered it after 2 denials lol