DOACs: What They Are, How They Work, and What You Need to Know
When you hear DOACs, Direct Oral Anticoagulants are a class of blood-thinning medications used to prevent dangerous clots without the need for regular blood tests. Also known as novel oral anticoagulants, they’ve replaced warfarin for millions of people with atrial fibrillation, deep vein thrombosis, or after hip or knee surgery. Unlike warfarin, which requires constant monitoring and strict diet limits, DOACs work with predictable dosing—no weekly INR checks, no avoiding leafy greens. That’s why they’re now the first choice for most patients needing long-term anticoagulation.
But DOACs aren’t one-size-fits-all. Atrial fibrillation, a common heart rhythm disorder that increases stroke risk by five times. is the top reason people start DOACs. Drugs like apixaban, rivaroxaban, and dabigatran each have slightly different profiles—some are better for kidney patients, others for those with a history of stomach bleeding. And while they’re safer than warfarin overall, they still carry risks. Bleeding can happen without warning, especially in older adults or those with liver or kidney problems. That’s why knowing your body’s limits matters more than ever.
Another key player here is blood thinners, a broad category that includes both older drugs like warfarin and newer ones like DOACs. But not all blood thinners are created equal. DOACs don’t need vitamin K adjustments, don’t interact as badly with most foods, and have fewer drug interactions than warfarin. Still, they can clash with certain antibiotics, antifungals, or even some seizure meds. If you’re on multiple prescriptions, that’s something your pharmacist needs to know. And if you’re over 75, have low body weight, or take NSAIDs for joint pain, your bleeding risk goes up—fast.
What you won’t find in most doctor’s office brochures are the real-life trade-offs. People on DOACs report fewer headaches and less anxiety about diet mistakes. But they also worry about what happens if they miss a dose, or if they fall and hit their head. Emergency rooms don’t always have reversal agents on hand, and not all hospitals stock them. That’s why keeping a printed list of your meds—including the exact name and dose of your DOAC—isn’t just smart, it’s life-saving.
Below, you’ll find real-world stories and science-backed facts about DOACs and the conditions they treat. From how they affect kidney function to how they interact with other common drugs like trimethoprim or SGLT2 inhibitors, we cover what actually matters when you’re taking them daily. No fluff. No jargon. Just what you need to stay safe, informed, and in control.
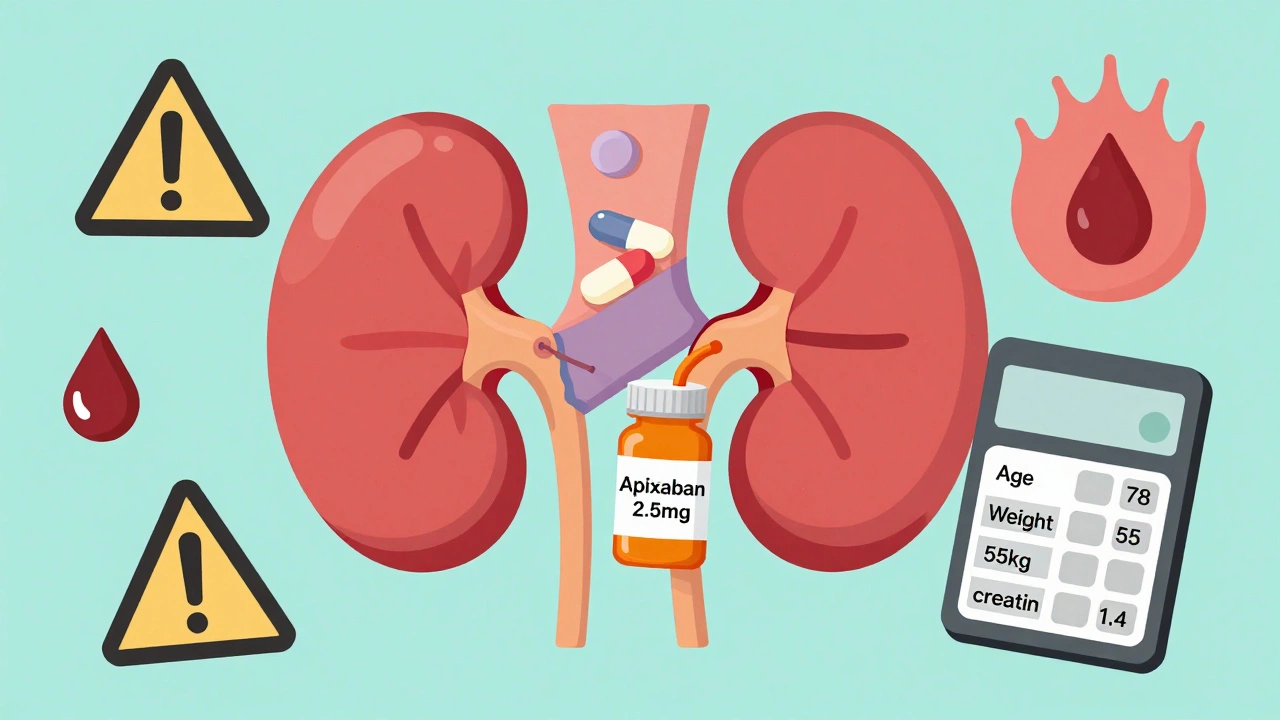
DOACs in Renal Impairment: How to Adjust Doses to Prevent Bleeding and Clots
- Dec, 1 2025
- 13
DOACs like apixaban and rivaroxaban are common blood thinners, but kidney problems require precise dose adjustments to prevent bleeding or clots. Learn the rules for safe use.
Categories
- Medication Information (113)
- Health and Wellness (52)
- Women's Health (6)
- Support Resources (5)
- Supplements (5)
- Pharmacy Reviews (5)
- Dermatology (4)
- Mental Health (4)
- Nutrition (3)
- Fitness and Wellness (3)
Archives
- February 2026 (12)
- January 2026 (27)
- December 2025 (30)
- November 2025 (24)
- October 2025 (29)
- September 2025 (14)
- August 2025 (2)
- July 2025 (7)
- June 2025 (2)
- May 2025 (3)
- April 2025 (4)
- March 2025 (3)
- online pharmacy
- dietary supplement
- medication safety
- health benefits
- side effects
- generic drugs
- drug interactions
- treatment
- wellness
- optimal health
- diabetes management
- safe medication purchase
- online pharmacy Australia
- brand name drugs
- authorized generics
- generic medications
- link
- women's health
- dietary supplements
- sleep
