DOACs in Renal Impairment: How to Adjust Doses to Prevent Bleeding and Clots
 Dec, 1 2025
Dec, 1 2025
DOAC Dosing Calculator for Kidney Impairment
Calculate Your CrCl
How to Take This Result
This calculator uses the Cockcroft-Gault formula, which is the FDA-recommended method for DOAC dosing. The eGFR is not accurate for DOAC dosing in kidney impairment.
Your CrCl Result
Calculate your CrCl to see result here
Why DOACs Need Special Care in Kidney Problems
Direct Oral Anticoagulants, or DOACs, are the most common blood thinners prescribed today for people with atrial fibrillation to prevent strokes. But if your kidneys aren’t working well, taking the wrong dose can be dangerous. Too much can cause life-threatening bleeding. Too little might let a clot form and trigger a stroke. The problem isn’t that DOACs don’t work - it’s that they’re cleared by your kidneys. If those kidneys are damaged, the drug builds up in your body. And unlike warfarin, you can’t just check a blood number to see if it’s safe.
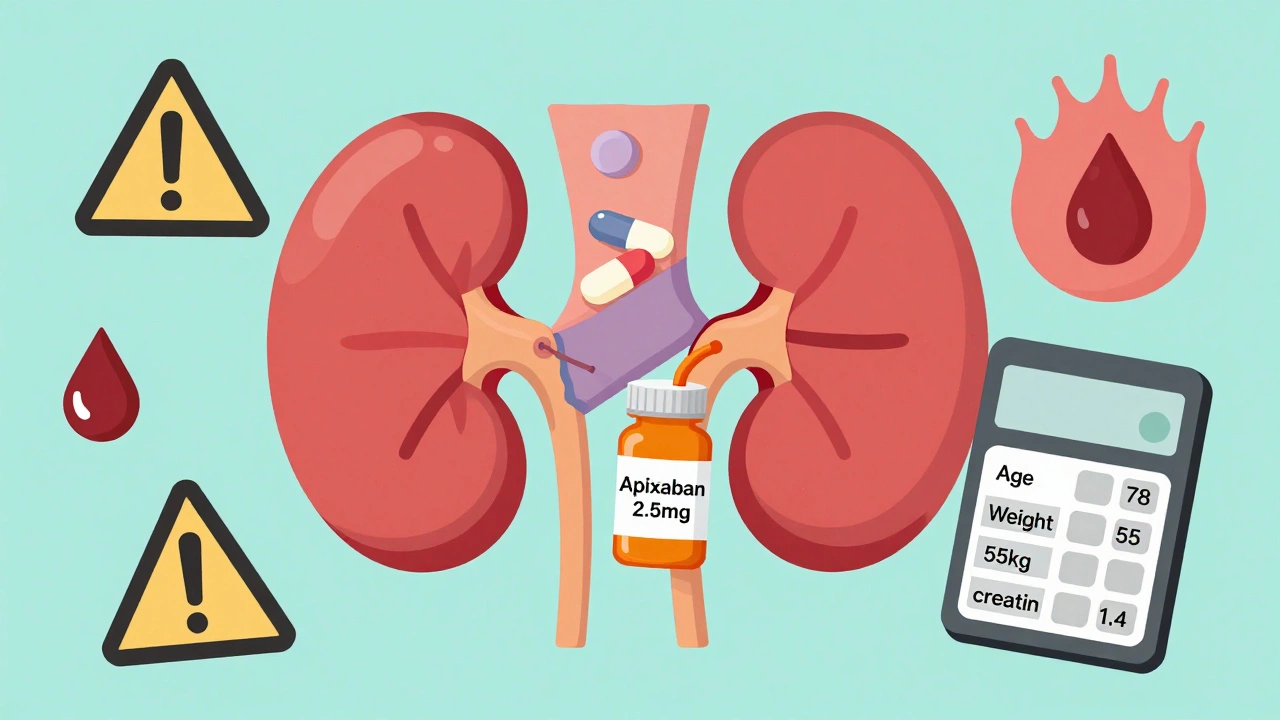
By 2023, over 87% of people with atrial fibrillation in the U.S. were on DOACs instead of warfarin. But nearly half of those patients also have chronic kidney disease. That’s a big overlap. And if you’re over 70, weigh less than 60 kg, or have high creatinine levels, your risk of side effects goes up even more. The key isn’t avoiding DOACs - it’s adjusting them right.
How to Measure Kidney Function for DOAC Dosing
Don’t use your eGFR number to decide your DOAC dose. That’s the most common mistake. Doctors and pharmacists often look at eGFR because it’s printed on lab reports. But for DOACs, you need creatinine clearance (CrCl) - calculated with the Cockcroft-Gault formula. This formula uses your age, weight, sex, and serum creatinine. It’s old, yes - developed in 1976 - but it’s still the gold standard. The FDA has required its use since 1998 for drugs cleared by the kidneys.
Here’s the formula: CrCl = [(140 - age) × weight (kg) × (0.85 if female)] / (72 × serum creatinine). For example, a 78-year-old woman weighing 55 kg with a creatinine of 1.4 mg/dL has a CrCl of about 28 mL/min. That’s severe kidney impairment. Now you know you need to cut her DOAC dose.
Many hospitals now have apps or electronic health record alerts that auto-calculate CrCl. But if you’re managing this yourself, double-check. In people over 80 or with low muscle mass, eGFR can overestimate kidney function by up to 30%. That’s not just a number - it’s a risk of bleeding.
DOAC Dosing Rules: What Works for Each Drug
Each DOAC has different rules. You can’t treat them the same. Here’s what you need to know:
- Apixaban (Eliquis): Standard dose is 5 mg twice daily. Reduce to 2.5 mg twice daily if you meet at least two of these: age 80+, body weight ≤60 kg, or serum creatinine ≥133 μmol/L (1.5 mg/dL). It’s the only DOAC approved for use in patients on hemodialysis - but only at the reduced dose. Never use if CrCl is below 15 mL/min.
- Rivaroxaban (Xarelto): Standard dose is 20 mg once daily. Reduce to 15 mg once daily if CrCl is 15-49 mL/min. Do not use at all if CrCl is below 15 mL/min. It’s not safe for dialysis patients.
- Dabigatran (Pradaxa): Standard dose is 150 mg twice daily. Reduce to 75 mg twice daily if CrCl is 15-30 mL/min. Not approved for CrCl below 15 mL/min.
- Edoxaban (Savaysa): Standard dose is 60 mg once daily. Reduce to 30 mg once daily if CrCl is 15-50 mL/min. Not approved below 15 mL/min.
Apixaban is the safest bet for kidney problems. Studies show it causes less bleeding than warfarin even in patients on dialysis. One study tracked 127 dialysis patients on apixaban 2.5 mg twice daily - major bleeding happened in only 1.8% over 18 months. In the warfarin group, it was 3.7%. That’s a big difference.

What Happens When Dosing Goes Wrong
Errors are common. A 2022 study in JAMA Internal Medicine found that 37.2% of DOAC prescriptions in patients with kidney disease were dosed incorrectly. Some were too high. Others were too low. The results? Bleeding. Clots. Hospital stays.
One real case: a 78-year-old man on hemodialysis was prescribed standard-dose apixaban (5 mg twice daily). He didn’t meet the weight or age criteria - but his creatinine was high, and his CrCl was below 15. He ended up in the ER with a massive gastrointestinal bleed. He survived, but only because his family caught the mistake before the next dose.
Another problem: doctors forget the ABCs. That’s the easy trick for apixaban: Age ≥80, Body weight ≤60 kg, Creatinine ≥1.3 mg/dL. If two of these are true, reduce the dose. It’s simple. But in busy clinics, it’s often skipped.
When DOACs Aren’t the Right Choice
There are times when warfarin still makes sense. If your CrCl is below 15 mL/min and you’re on dialysis, DOACs aren’t fully approved. But warfarin isn’t perfect either. It causes more brain bleeds and vascular calcification in kidney patients. Still, some experts recommend warfarin in this group because we have more long-term data.
Here’s the bottom line: if your CrCl is below 15 mL/min, you’re in a gray zone. Apixaban at 2.5 mg twice daily is the best-supported option. Rivaroxaban, dabigatran, and edoxaban should be avoided. The 2023 KDIGO guidelines say evidence is still lacking - but that doesn’t mean you do nothing. You choose the safest available option.
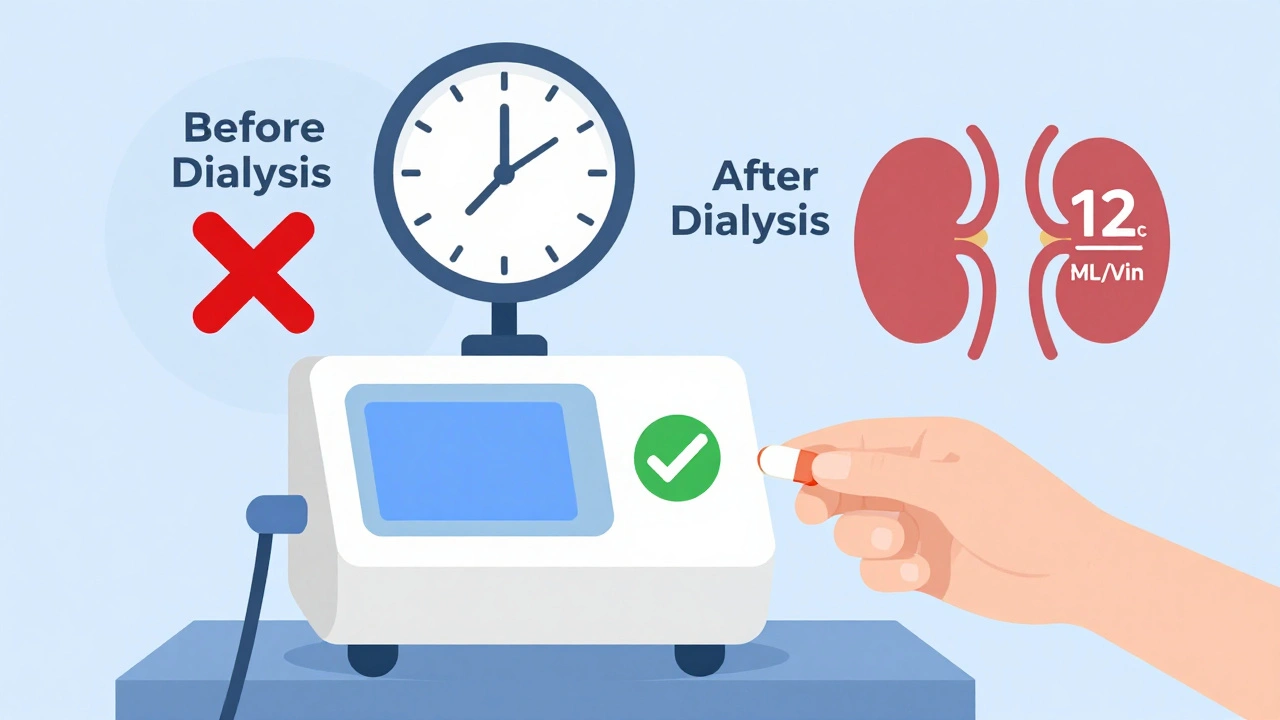
And if you’re on dialysis? You need to take your DOAC after the session, not before. Dialysis removes some of the drug. Taking it before dialysis means you get too little. Taking it after means you get the full dose. Timing matters.
What You Should Do Right Now
If you’re on a DOAC and have kidney disease, here’s what to do today:
- Ask your doctor or pharmacist to calculate your CrCl using the Cockcroft-Gault formula - not eGFR.
- Check your current DOAC dose against the rules above. Don’t assume your dose is right.
- If you’re over 75, weigh less than 60 kg, or have high creatinine, ask if you qualify for a reduced dose - especially for apixaban.
- Get your creatinine checked every 3-6 months if your kidney function is unstable. More often if you’re sick or on new medications.
- Ask about a virtual anticoagulation clinic. These services track your labs, adjust doses, and call you if something’s off. One study showed they cut adverse events by over 20%.
Don’t wait for a bleeding event to realize your dose was wrong. Many patients don’t feel anything until it’s too late. DOACs don’t cause dizziness or fatigue when they’re too high. They just silently increase your bleeding risk.
What’s Coming Next
More data is coming. The RENAL-AF trial, expected to finish in 2025, will compare apixaban to warfarin in patients with severe kidney disease. That might finally give us clear answers. For now, we work with what we have.
By 2026, experts predict we’ll have specific DOAC dosing rules for every stage of kidney disease - even dialysis. But until then, the safest approach is simple: use apixaban at the lowest effective dose, calculate CrCl properly, and check your labs often.
Frequently Asked Questions
Can I take a DOAC if I’m on dialysis?
Yes - but only apixaban, and only at the reduced dose of 2.5 mg twice daily. Rivaroxaban, dabigatran, and edoxaban are not recommended. Take apixaban after your dialysis session, not before. Dialysis removes some of the drug, so taking it after ensures you get the full dose.
Why can’t I just use eGFR instead of CrCl?
eGFR overestimates kidney function in older adults, people with low muscle mass, or those who are underweight. DOACs are cleared by the kidneys, and if you think your kidneys are working better than they are, you might take too high a dose. The Cockcroft-Gault formula is the only one approved by the FDA for DOAC dosing.
Is apixaban really safer than warfarin for kidney patients?
Yes, in most cases. Studies show apixaban causes fewer major bleeds than warfarin in patients with moderate to severe kidney disease. In dialysis patients, bleeding rates are lower with apixaban 2.5 mg twice daily than with warfarin. Warfarin also increases the risk of calcium buildup in blood vessels - a big problem in kidney disease.
What if I forget to take my DOAC because of dialysis?
If you miss a dose and it’s been less than 6 hours since your scheduled time, take it as soon as you remember. If it’s more than 6 hours, skip it and take your next dose at the regular time. Never double up. For patients on dialysis, always coordinate timing with your dialysis schedule - your pharmacist can help.
Can other medications affect my DOAC dose?
Yes. Drugs like ketoconazole, clarithromycin, or rifampin can change how your body processes DOACs. Even over-the-counter NSAIDs like ibuprofen can increase bleeding risk. Always tell your doctor and pharmacist about every medication you take - including herbs and supplements.
Final Thoughts
DOACs are better than warfarin for most people with atrial fibrillation - but only if used correctly. In kidney disease, the margin for error is small. A wrong dose doesn’t just mean a side effect - it can mean a stroke, a bleed, or death. The solution isn’t complicated: know your CrCl, follow the dosing rules, and choose apixaban when possible. Don’t rely on assumptions. Don’t skip the math. And never assume your dose is safe just because your doctor prescribed it. Ask. Double-check. Stay in control.

Conor Forde
December 3, 2025 AT 04:04Linda Migdal
December 3, 2025 AT 18:35Tommy Walton
December 5, 2025 AT 05:02James Steele
December 5, 2025 AT 22:45Louise Girvan
December 7, 2025 AT 03:50soorya Raju
December 7, 2025 AT 22:59Dennis Jesuyon Balogun
December 8, 2025 AT 18:47Grant Hurley
December 8, 2025 AT 21:34Lucinda Bresnehan
December 10, 2025 AT 10:56Shannon Gabrielle
December 11, 2025 AT 13:05ANN JACOBS
December 12, 2025 AT 17:56Nnaemeka Kingsley
December 12, 2025 AT 18:56Kshitij Shah
December 12, 2025 AT 23:43