Dizziness with Diabetes Meds: What You Need to Know
When you take dizziness with diabetes meds, a side effect that occurs when blood sugar drops too low or blood pressure shifts due to medication. Also known as lightheadedness from antidiabetic drugs, it’s not just "feeling off"—it’s your body signaling something needs attention. Many people assume dizziness is just part of aging or stress, but when it shows up after taking metformin, sulfonylureas, or SGLT2 inhibitors like dapagliflozin, it’s often tied to hypoglycemia, a dangerous drop in blood sugar that happens when meds outpace food intake or activity. This isn’t rare: studies show nearly 1 in 3 people on insulin or sulfonylureas experience at least one episode a year. And it’s not just sugar—some diabetes drugs also affect blood pressure, especially when combined with blood pressure meds, like ACE inhibitors or diuretics, which can amplify fluid shifts and cause orthostatic dizziness.
Dizziness isn’t always a sign you’re taking too much. Sometimes it’s the opposite—your body’s adjusting to better glucose control. When your blood sugar stays high for months, your brain gets used to it. Suddenly lowering it can make you feel dizzy even if your sugar is now in the normal range. That’s called "relative hypoglycemia," and it’s why some people feel awful when their A1C drops from 9% to 7%. It’s not low enough to be dangerous, but your body doesn’t know that yet. Also, if you’re on multiple meds for diabetes, heart disease, or kidney issues, you’re at higher risk for drug-disease interactions, where one medication worsens another condition, like a blood pressure pill making dizziness worse in someone with nerve damage from diabetes. These hidden clashes are why keeping a log of when you feel dizzy—along with your last meal, activity, and meds taken—is so important.
What you do next matters more than you think. Stopping your meds on your own can lead to high blood sugar, which brings its own risks. Instead, track the pattern: does it happen mostly in the morning? After exercise? When you skip a meal? That info helps your doctor adjust timing, dosage, or even switch you to a drug less likely to cause drops. Some people find switching from glimepiride to sitagliptin reduces dizziness because it doesn’t force insulin release. Others benefit from splitting doses or adding a snack before bed. And if you’re on a diuretic for heart issues, your doctor might check your electrolytes—low sodium or potassium can make dizziness worse. You don’t have to live with this feeling. The right fix is often simple, but it starts with knowing what’s really going on.
Below, you’ll find real-world insights from people who’ve dealt with this exact issue—what worked, what didn’t, and how they got their balance back without giving up their diabetes treatment.
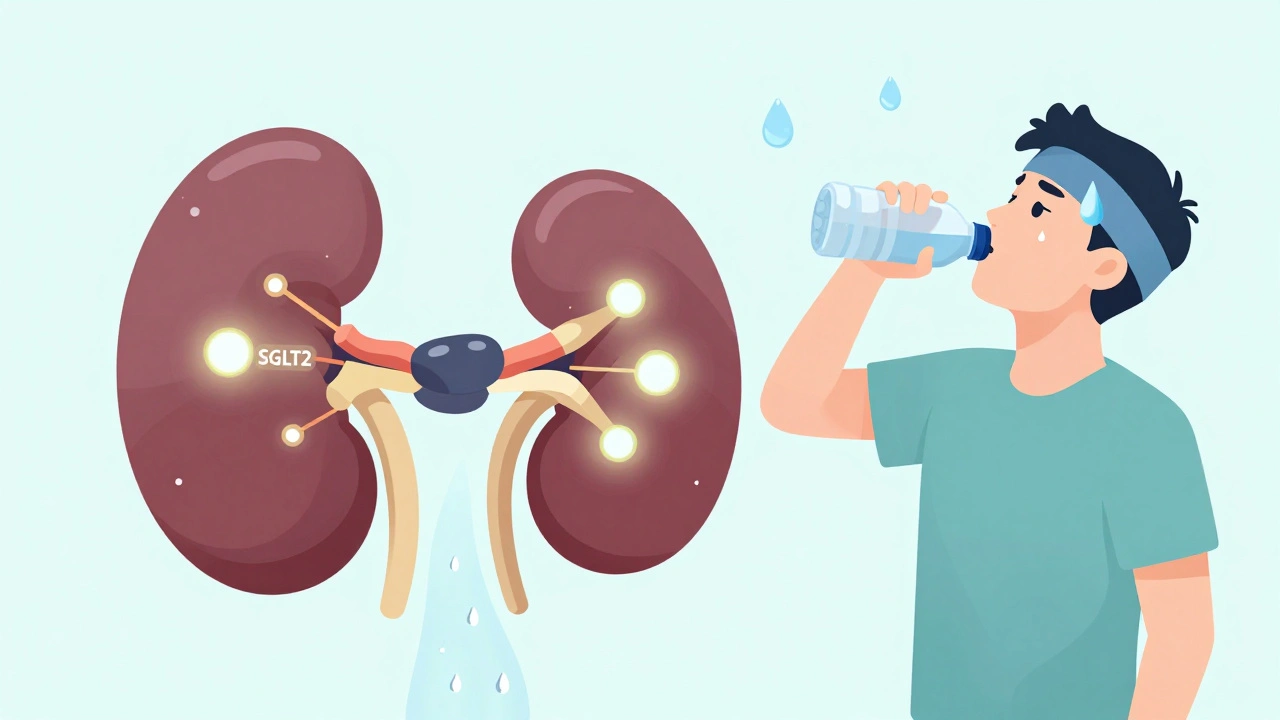
SGLT2 Inhibitor Side Effects: Dehydration, Dizziness, and Blood Pressure Changes Explained
- Dec, 1 2025
- 15
SGLT2 inhibitors help lower blood sugar and protect the heart and kidneys, but they can cause dehydration, dizziness, and low blood pressure. Learn who’s at risk and how to stay safe while taking them.
Categories
- Medication Information (113)
- Health and Wellness (52)
- Women's Health (6)
- Support Resources (5)
- Supplements (5)
- Pharmacy Reviews (5)
- Dermatology (4)
- Mental Health (4)
- Nutrition (3)
- Fitness and Wellness (3)
Archives
- February 2026 (12)
- January 2026 (27)
- December 2025 (30)
- November 2025 (24)
- October 2025 (29)
- September 2025 (14)
- August 2025 (2)
- July 2025 (7)
- June 2025 (2)
- May 2025 (3)
- April 2025 (4)
- March 2025 (3)
- online pharmacy
- dietary supplement
- medication safety
- health benefits
- side effects
- generic drugs
- drug interactions
- treatment
- wellness
- optimal health
- diabetes management
- safe medication purchase
- online pharmacy Australia
- brand name drugs
- authorized generics
- generic medications
- link
- women's health
- dietary supplements
- sleep
