Dehydration from SGLT2 Inhibitors: Risks, Signs, and What to Do
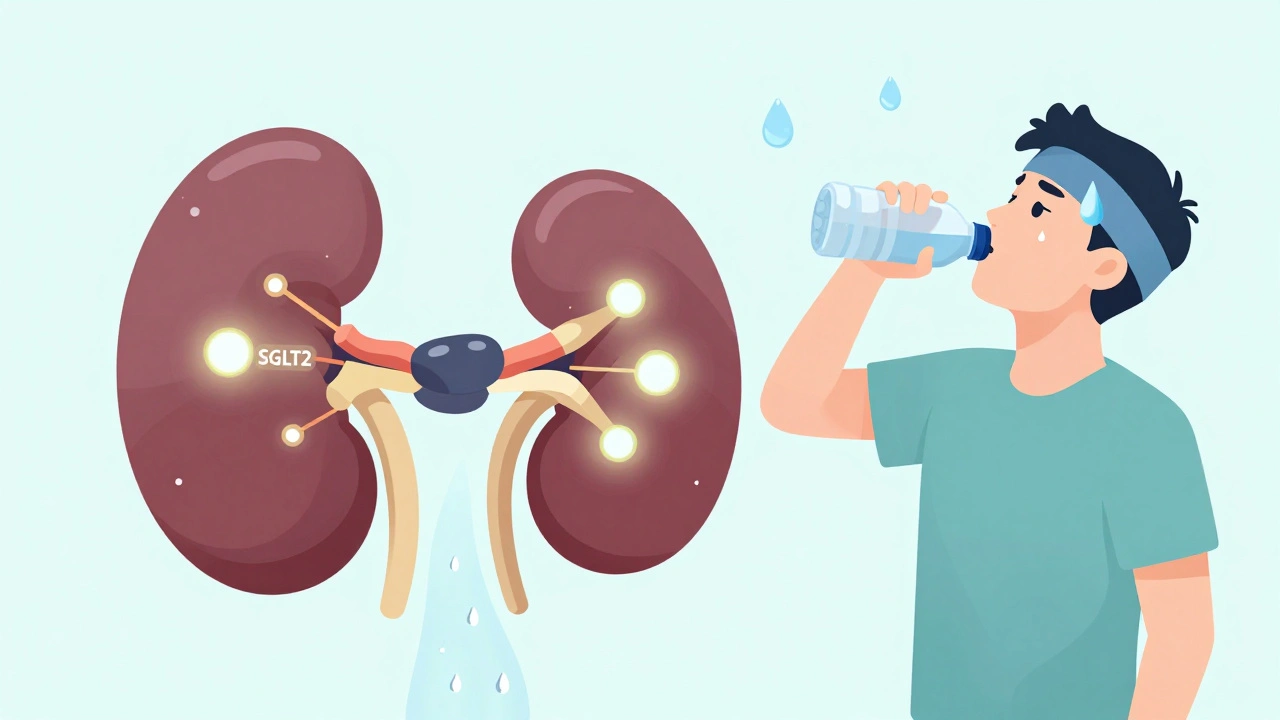
When you take an SGLT2 inhibitor, a class of diabetes medications that make your kidneys flush out excess sugar through urine. Also known as gliflozins, these drugs help lower blood sugar—but they also pull water out with it, which can leave you dangerously dehydrated even if your sugar levels seem fine. This isn’t just about feeling thirsty. It’s about your body losing fluids faster than you can replace them, and that’s when things get serious.
Dehydration from SGLT2 inhibitors, medications like dapagliflozin, empagliflozin, and canagliflozin that block sugar reabsorption in the kidneys happens because these drugs force your body to pee out up to 100 grams of sugar a day. That sugar drags water with it—sometimes over a liter extra per day. You might not notice until you’re already low on fluids. Older adults, people on diuretics, those with kidney issues, or anyone cutting carbs or alcohol are at higher risk. And here’s the twist: you can get euglycemic DKA, a life-threatening condition where your body starts burning fat for fuel despite normal blood sugar—because the fluid loss and stress trigger ketones, even when your glucose looks okay.
This isn’t rare. Studies show up to 1 in 20 people on these drugs develop signs of dehydration within the first few months. Symptoms? Dry mouth, dizziness when standing, dark urine, fatigue, confusion, or a rapid heartbeat. Some people mistake it for the flu. Others think their blood sugar is under control, so they ignore it. But if you’re on one of these meds and you’re sweating more than usual, skipping meals, or getting sick with vomiting or diarrhea, your risk spikes. You need to drink more water—not just when you’re thirsty, but regularly. And if you’re scheduled for surgery or a scan that requires fasting, talk to your doctor about pausing the drug.
What makes this tricky is that SGLT2 inhibitors are great for heart and kidney protection in people with type 2 diabetes. But that benefit only works if you’re not dehydrated. The same mechanism that helps your heart also stresses your kidneys. It’s why doctors now check your kidney function and fluid status before starting these drugs—and why you should never stop drinking water just because you’re not thirsty.
Below, you’ll find real patient stories, medical guidelines, and safety tips from posts that dig into how these drugs affect your body beyond blood sugar. You’ll learn how to spot early warning signs, what tests your doctor should run, and how to balance the benefits with the risks—without guessing.
SGLT2 Inhibitor Side Effects: Dehydration, Dizziness, and Blood Pressure Changes Explained
- Dec, 1 2025
- 15
SGLT2 inhibitors help lower blood sugar and protect the heart and kidneys, but they can cause dehydration, dizziness, and low blood pressure. Learn who’s at risk and how to stay safe while taking them.
Categories
- Medication Information (113)
- Health and Wellness (52)
- Women's Health (6)
- Support Resources (5)
- Supplements (5)
- Pharmacy Reviews (5)
- Dermatology (4)
- Mental Health (4)
- Nutrition (3)
- Fitness and Wellness (3)
Archives
- February 2026 (12)
- January 2026 (27)
- December 2025 (30)
- November 2025 (24)
- October 2025 (29)
- September 2025 (14)
- August 2025 (2)
- July 2025 (7)
- June 2025 (2)
- May 2025 (3)
- April 2025 (4)
- March 2025 (3)
- online pharmacy
- dietary supplement
- medication safety
- health benefits
- side effects
- generic drugs
- drug interactions
- treatment
- wellness
- optimal health
- diabetes management
- safe medication purchase
- online pharmacy Australia
- brand name drugs
- authorized generics
- generic medications
- link
- women's health
- dietary supplements
- sleep
