Conjugated Estrogens: What They Are, How They Work, and What You Need to Know
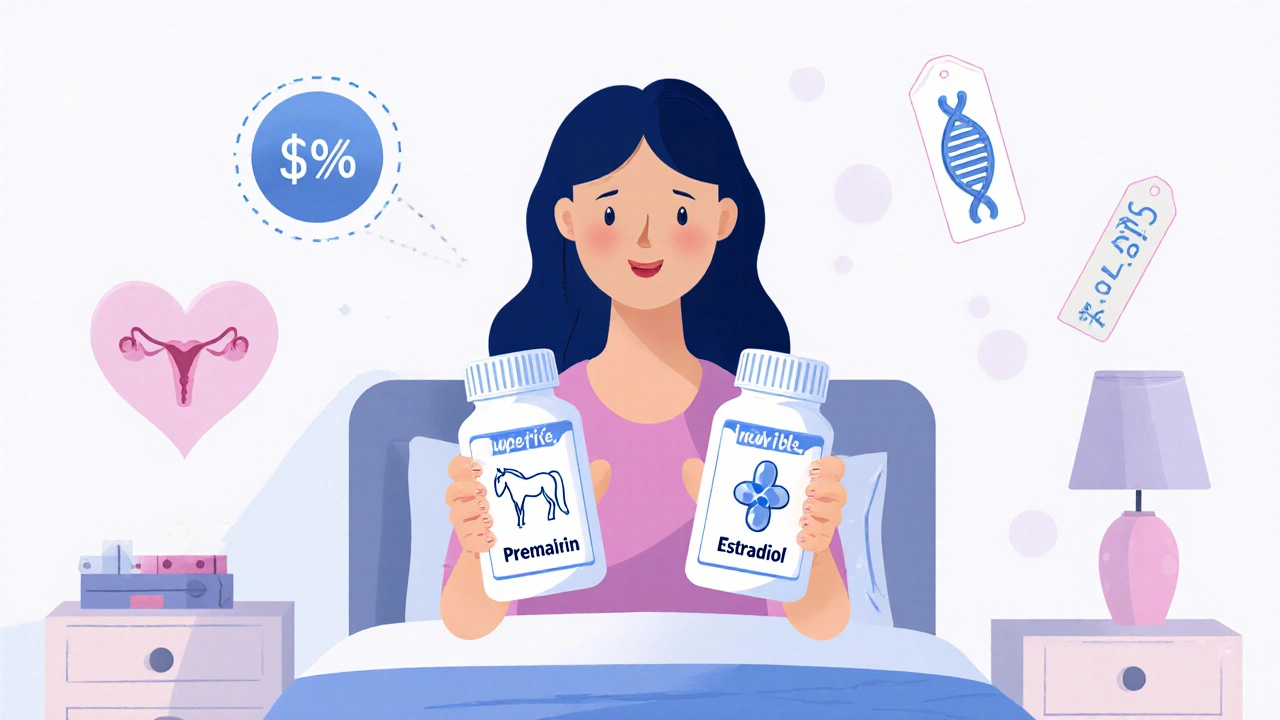
When your body stops making enough estrogen after menopause, symptoms like hot flashes, night sweats, and vaginal dryness can make daily life harder. Conjugated estrogens, a mix of estrogen hormones derived from pregnant mare urine, used to replace declining natural estrogen levels in postmenopausal women. Also known as Premarin, it’s one of the most prescribed forms of hormone therapy in the UK for women dealing with moderate to severe menopause symptoms. Unlike synthetic estrogens, conjugated estrogens contain a blend of different estrogen types—some naturally occurring in humans, others not—which affects how your body responds to them.
They’re not just for hot flashes. Doctors often prescribe conjugated estrogens to help prevent bone loss in women at risk for osteoporosis, especially if they can’t take other bone-strengthening meds. But they’re not a one-size-fits-all solution. Women with a history of breast cancer, blood clots, liver disease, or unexplained vaginal bleeding are usually advised against them. And if you still have a uterus, you’ll need to take progesterone along with it to lower the risk of uterine cancer. This combo is called hormone replacement therapy, or HRT, and it’s a balancing act—relieving symptoms while minimizing risks.
People often wonder how conjugated estrogens compare to other estrogen options, like estradiol pills or patches. The main difference is how they’re made and how your body processes them. Conjugated estrogens are taken orally, which means your liver breaks them down first—this can affect cholesterol and clotting risks more than skin-applied forms. That’s why some women and their doctors choose transdermal patches or gels instead. It’s not about which is "better," but which fits your health profile, lifestyle, and personal comfort.
Side effects aren’t rare. Bloating, breast tenderness, headaches, and mood swings are common in the first few months. For some, they fade. For others, they mean switching formulas or doses. It’s not just about taking a pill—it’s about monitoring how your body reacts over time. Regular check-ups with your doctor, blood pressure checks, and breast exams are part of the process. And while some online sources push conjugated estrogens as a "miracle cure," the science doesn’t back that up. It’s a tool, not a fix.
What you’ll find in the posts below isn’t a list of ads or generic advice. It’s real, practical information from people who’ve walked this path. You’ll see how women manage side effects, what alternatives they tried, how timing and dosage made a difference, and how some chose to stop altogether. There’s no single right answer—but there are smart choices. And that’s what this collection is built to help you find.
Compare Premarin (Conjugated Estrogens) with Alternatives: What Works Best in 2025
- Oct, 28 2025
- 14
Compare Premarin with safer, more affordable alternatives like estradiol, vaginal estrogen, and non-hormonal options for menopause symptoms in 2025. Learn what works best and how to choose.
Categories
- Medication Information (111)
- Health and Wellness (52)
- Women's Health (6)
- Support Resources (5)
- Supplements (5)
- Pharmacy Reviews (5)
- Dermatology (4)
- Mental Health (4)
- Nutrition (3)
- Fitness and Wellness (3)
Archives
- February 2026 (10)
- January 2026 (27)
- December 2025 (30)
- November 2025 (24)
- October 2025 (29)
- September 2025 (14)
- August 2025 (2)
- July 2025 (7)
- June 2025 (2)
- May 2025 (3)
- April 2025 (4)
- March 2025 (3)
- online pharmacy
- dietary supplement
- medication safety
- health benefits
- side effects
- generic drugs
- treatment
- wellness
- optimal health
- diabetes management
- safe medication purchase
- online pharmacy Australia
- brand name drugs
- drug interactions
- authorized generics
- generic medications
- link
- women's health
- dietary supplements
- sleep
