Time in Range: How CGM Metrics Help You Manage Diabetes Daily
 Jan, 15 2026
Jan, 15 2026
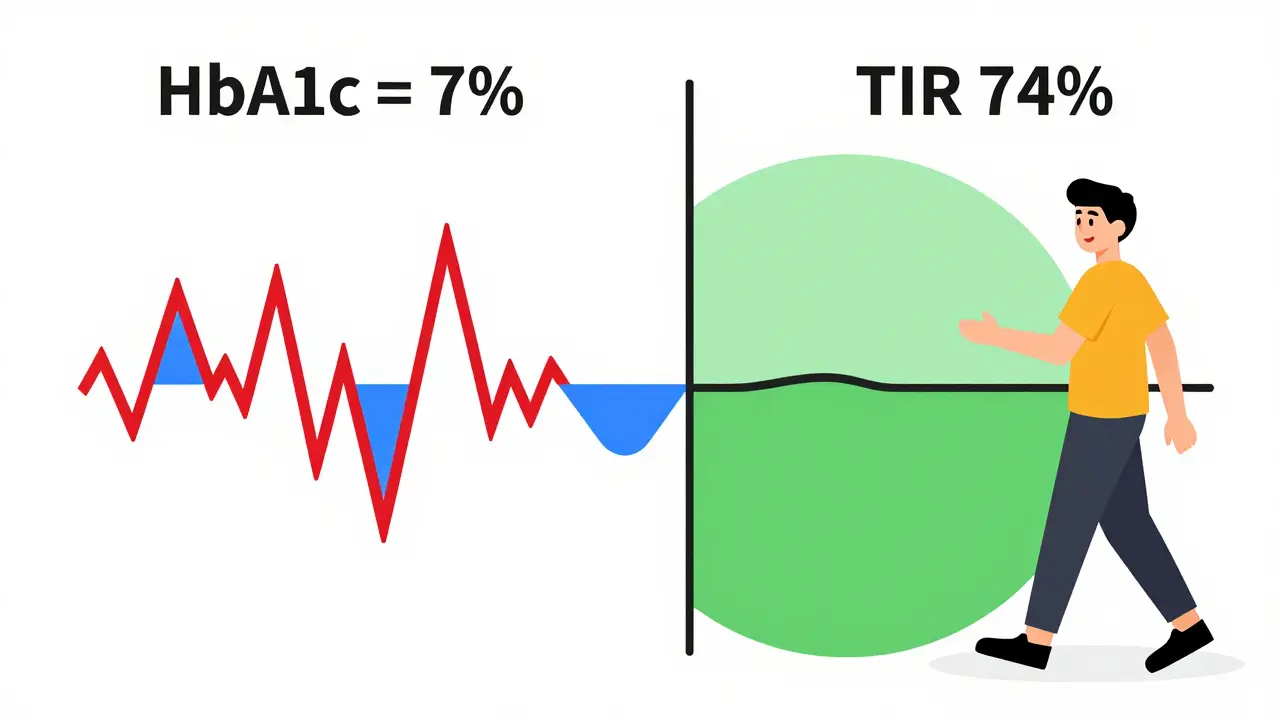
Most people with diabetes know their HbA1c number. It’s the lab test that tells you your average blood sugar over the last three months. But here’s the problem: two people can have the same HbA1c - say, 7% - and one could be spending most of their day with dangerous highs and lows, while the other stays steady. That’s where time in range changes everything.
What Time in Range Really Means
Time in range (TIR) isn’t a fancy term - it’s simple. It’s the percentage of time your blood glucose stays between 70 and 180 mg/dL (3.9 to 10.0 mmol/L). That’s the sweet spot. Not too high, not too low. Most experts agree you should aim for at least 70% of your day - about 17 hours - in that range. For someone using a continuous glucose monitor (CGM), that’s not a guess. It’s a fact. CGMs check your glucose every 5 minutes, giving you over 1,300 data points in just two weeks. That’s more than a thousand snapshots of your body’s response to food, sleep, stress, and movement.
Before CGMs, we only had HbA1c. Think of HbA1c like reading the summary of a book. You know the ending, but you miss all the drama in between. TIR is reading the whole book. You see when your sugar spikes after lunch. You notice the dip after evening walks. You catch the 3 a.m. crash you never knew about.
Why TIR Beats HbA1c for Daily Life
HbA1c doesn’t tell you if you’re having five hypoglycemic episodes a week. It doesn’t show you that your blood sugar rockets to 220 mg/dL every time you eat oatmeal. It hides the peaks and valleys. That’s dangerous. Hypoglycemia can lead to falls, confusion, even seizures. Chronic hyperglycemia increases your risk of nerve damage, kidney disease, and vision problems.
Studies show that for every 10% increase in time in range, your risk of complications drops significantly. A 2025 study in the Journal of Clinical Endocrinology & Metabolism found that people who spent more than 70% of their day in range had 40% fewer hospital visits for glucose-related emergencies than those who didn’t - even when their HbA1c was the same.
And here’s the kicker: you can improve your TIR without changing your HbA1c target. You don’t need to chase a 6% A1c. You just need to smooth out the ride. That’s why the American Diabetes Association’s 2025 Standards of Care now say CGM and TIR should be considered for everyone with type 2 diabetes on glucose-lowering meds - not just insulin users.
The Other Numbers That Matter
TIR isn’t the only metric. It’s part of a bigger picture. Your CGM also tracks:
- Time Below Range (TBR): Time spent under 70 mg/dL. Aim for less than 4% of the day. Less than 1% should be under 54 mg/dL - that’s severe hypoglycemia.
- Time Above Range (TAR): Time over 180 mg/dL. You want this under 25%. The lower, the better.
- Glucose Variability: How much your numbers swing. High variability means more stress on your body, even if your average looks fine.
One patient I worked with in Sydney had an HbA1c of 6.9% - great, right? But his TIR was only 52%. He was spending nearly 8 hours a day above 180 and over 2 hours below 70. He thought he was doing well. His CGM showed he was playing Russian roulette with his health. After adjusting his evening snack and timing his metformin, his TIR jumped to 74% in six weeks. His HbA1c didn’t change much - but his life did.
How to Use TIR Data in Real Life
Having the data is useless if you don’t act on it. Here’s how to turn numbers into action:
- Look for patterns. Are your numbers high every Monday morning? Maybe you’re eating more carbs over the weekend. Are you crashing after 3 p.m.? Maybe your lunch is too heavy on refined carbs.
- Test one thing at a time. Don’t change your diet, exercise, and meds all at once. Try swapping white rice for quinoa for three days. See what happens.
- Use your CGM’s alerts. Set low and high alerts. You’ll catch trends before they become crises.
- Share your reports. Don’t just show your doctor your HbA1c. Bring your 14-day CGM report. Highlight the spikes, the dips, the good days. Ask: “What’s causing this?”
One woman in Melbourne discovered her “healthy” granola bar spiked her glucose to 210 mg/dL. She’d been eating it for years thinking it was good for her. With TIR, she found a better option - and saved herself from years of hidden damage.
Getting Started with CGM
If you’re not using a CGM yet, here’s what you need to know:
- Wear time matters. You need at least 70% of your CGM sensor active to get reliable TIR data. That means 10+ days out of a 14-day wear period.
- It’s not just for insulin users. The 2025 ADA guidelines now support CGM for anyone with type 2 diabetes on metformin, SGLT2 inhibitors, GLP-1s, or other glucose-lowering drugs.
- Insurance coverage is improving. In the U.S., Medicare now covers CGM for type 2 patients meeting certain criteria. In Australia, private insurers are starting to follow suit. Check with your provider.
- Don’t skip education. Your diabetes educator can help you interpret the graphs. Don’t try to decode the spikes alone.
CGM devices from Dexcom, Abbott, and Medtronic are more accurate and affordable than ever. The market grew from $4.8 billion in 2022 to an estimated $18.6 billion by 2030 - not because of hype, but because people are seeing results.

What’s Next for Time in Range?
Researchers are now looking at “time in tight range” - staying between 70 and 140 mg/dL. That’s the range most people without diabetes stay in. It’s harder to achieve, but early data suggests it may lower long-term risks even more.
Artificial intelligence is starting to predict your glucose spikes before they happen. One system in development can tell you, “Your sugar will rise in 45 minutes if you eat that pasta. Try adding vinegar to your meal.” That’s not sci-fi - it’s coming fast.
The goal isn’t perfection. It’s progress. You don’t need to be in range 100% of the time. You just need to be in range more than you’re out. Every extra hour you spend in range is an hour your body isn’t under stress.
Final Thought: Your Body Tells You Everything
For decades, diabetes care was based on averages. We measured once a quarter. We made decisions in the dark. Now, we have real-time feedback. Your body is talking. CGM and TIR are the tools that let you listen.
You don’t need to be perfect. You just need to be aware. And with TIR, you’re no longer guessing what’s happening between your doctor visits. You’re in control - one glucose reading at a time.
What is a good Time in Range percentage for type 2 diabetes?
A good Time in Range (TIR) target for most adults with type 2 diabetes is at least 70% of the day, meaning your glucose stays between 70 and 180 mg/dL (3.9-10.0 mmol/L) for 17 or more hours daily. This aligns with the American Diabetes Association’s 2025 guidelines and corresponds to an HbA1c of about 7%. Some people may aim for higher targets, like 75% or more, depending on their health goals and risk of hypoglycemia.
Can I improve my TIR without changing my medications?
Yes. Many people improve their TIR through lifestyle changes alone. Adjusting meal timing, choosing lower-glycemic foods, walking after meals, and managing stress can all have a big impact. One study showed that a 15-minute walk after dinner reduced post-meal spikes by up to 30%. You don’t always need more drugs - you need better timing and smarter choices.
How often should I wear my CGM to get accurate TIR data?
For reliable TIR results, wear your CGM for at least 14 days and ensure it’s active (sending data) for at least 70% of that time - that’s about 10 days or more. Shorter periods can give you a snapshot, but 14 days captures weekend patterns, stress days, and meals you might skip during the week. The International Consensus on CGM Metrics recommends this minimum for clinical use.
Is TIR more important than HbA1c?
They’re not competitors - they’re partners. HbA1c still matters as a long-term average. But TIR tells you what’s happening day-to-day. Two people can have the same HbA1c but wildly different TIR. One might be stable and safe; the other could be in danger of lows or highs. TIR gives you the details HbA1c hides. Use both together for the full picture.
Do I need a prescription to get a CGM for type 2 diabetes?
In most cases, yes. CGMs are medical devices and require a prescription in Australia, the U.S., and many other countries. However, the 2025 ADA guidelines now recommend CGM for adults with type 2 diabetes on glucose-lowering medications - even if they’re not on insulin. Talk to your doctor about whether you qualify, especially if you’re having unexplained highs or lows.
What if my CGM shows I’m in range most of the time but still feel tired or foggy?
You might be experiencing glucose variability - big swings even within the target range. A CGM can show you if your numbers are jumping from 170 to 80 in an hour. That rollercoaster can cause fatigue, brain fog, and irritability even if you’re technically “in range.” Look at your coefficient of variation (CV) on your CGM report. If it’s above 36%, your variability is high. Try eating more protein and fiber with meals, and avoid large carb loads.

Joie Cregin
January 16, 2026 AT 03:06Okay but can we talk about how life-changing this is? I used to think my A1c was my whole story - turns out I was just surviving, not living. My CGM showed I was crashing at 3 a.m. every night like clockwork. No one told me that was even possible. Now I eat a handful of almonds before bed and suddenly I’m not waking up drenched in sweat, heart racing like I just ran a marathon. It’s wild how much your body tells you if you just stop ignoring the noise.
Melodie Lesesne
January 17, 2026 AT 17:25I love this so much. I started using a CGM last year after my doc said ‘just keep taking metformin and eat less sugar’ - like that’s helpful. Turns out my ‘healthy’ oatmeal was turning me into a glucose volcano. Now I swap it for eggs and avocado. My TIR went from 48% to 76% in two months. No new meds. Just data. And honestly? It feels like I got my life back.
Corey Sawchuk
January 19, 2026 AT 00:18Been using Dexcom for 18 months. The biggest shift wasn’t the numbers - it was the awareness. You stop guessing. You stop feeling guilty. You start making choices based on real feedback. I used to blame stress for my highs. Turns out it was the iced tea I thought was ‘diet friendly.’ One small fix. Huge difference.
Stephen Tulloch
January 20, 2026 AT 23:30Ugh I’m so tired of people acting like CGMs are some magical cure 🤡 HbA1c still matters. You think you’re ‘in range’ but if your average is still 8.5? Congrats you’re just less chaotic about being diabetic. Also most people don’t even understand their own data. I’ve seen folks get paranoid over a 160 spike like it’s a death sentence. Chill. It’s one number. Not your soul.
Bianca Leonhardt
January 22, 2026 AT 06:43Let’s be real - if you need a CGM to know what happens after you eat a bagel, maybe you shouldn’t be eating bagels. This isn’t rocket science. It’s basic nutrition. Stop outsourcing your brain to a device and learn to listen to your body. Also, 70% TIR? That’s barely above average. If you’re not hitting 80%+ you’re still playing with fire.
Travis Craw
January 22, 2026 AT 12:20so i got a cgm last month and wow. i had no idea my coffee with half and half was spiking me to 200. i thought it was just ‘normal’. now i drink it black and my afternoons dont feel like i’m dragging a couch. also the alerts are kinda scary at first but then you get used to it. like a little beep saying ‘hey your body is talking’.
Christina Bilotti
January 22, 2026 AT 19:52Oh sweetie. You think you’re ‘in range’? Let me guess - you’re eating ‘gluten-free granola’ and calling it healthy? 😂 That stuff is just sugar with a fancy label. My CGM showed my ‘healthy’ smoothie spiked me to 240. I cried. Then I threw it out. If you’re not tracking variability and not aiming for 80%+ TIR, you’re not managing diabetes. You’re just delaying the inevitable. Stop celebrating 70%. That’s the bare minimum.
Henry Ip
January 24, 2026 AT 11:08One thing I wish more people talked about - it’s not about perfection. Some days I’m at 65%. That’s okay. What matters is the trend. I track weekly averages now, not daily panic. And I’ve learned to celebrate the small wins - like walking after dinner and seeing my spike drop 40 points. That’s power. Not magic. Just consistency. You got this.
Jody Fahrenkrug
January 26, 2026 AT 02:05My doctor finally got it after I showed him my 14-day report. He said, ‘I’ve been looking at your A1c for years. I never knew you were doing this much damage between visits.’ Now he asks for my CGM data before every appointment. It’s weird - for the first time, I feel like my care team actually sees me.