Sleep and Mental Health: How Treating Insomnia Helps with Depression and Anxiety
 Dec, 17 2025
Dec, 17 2025
When you can’t sleep, your mind doesn’t rest. It races. It replays conversations. It fears tomorrow. For people with depression or anxiety, insomnia isn’t just a side effect-it’s fuel. And treating it can change everything.
Insomnia Isn’t Just a Symptom-It’s a Driver
Many people think trouble sleeping comes from being depressed or anxious. That’s partly true. But research now shows the opposite is also true: chronic insomnia doesn’t just follow mental illness-it helps create it. A 2025 study in Frontiers in Psychiatry found that people with long-term insomnia are 40 times more likely to develop severe depression than those who sleep well. That’s not a coincidence. It’s a pattern.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), published in 2013, was the first to officially recognize insomnia as its own condition-not just a symptom. This shift changed how doctors think about treatment. If you treat depression but ignore the sleep problems, you’re leaving the fire burning while you try to put out the smoke.
Why CBT-I Is the Gold Standard
The most effective treatment for insomnia linked to depression and anxiety isn’t a pill. It’s Cognitive Behavioral Therapy for Insomnia, or CBT-I. Unlike sleeping pills that offer quick relief but no long-term change, CBT-I rewires the thoughts and habits keeping you awake.
CBT-I isn’t one thing. It’s a mix of four proven strategies:
- Stimulus control: Your bed is only for sleep and sex-not scrolling, worrying, or watching TV. If you’re not asleep in 20 minutes, get up and go to another room until you feel sleepy.
- Sleep restriction: You’re spending too much time in bed awake. This method cuts your time in bed to match how much you’re actually sleeping-even if it’s only 5 hours. It sounds harsh, but it rebuilds your body’s sleep drive.
- Relaxation techniques: Deep breathing, progressive muscle relaxation, and mindfulness calm the nervous system. Your body can’t be tense and asleep at the same time.
- Cognitive therapy: You believe you need 8 hours to function, or that one bad night will ruin your week. These thoughts keep you alert. CBT-I helps you replace them with facts.
Most programs run for 6 to 8 weeks, with weekly 50-minute sessions. But now, digital versions like Sleepio and SHUTi deliver the same results through apps. One study showed a 57% drop in the odds of moderate-to-severe depression among users of these platforms compared to people who just read sleep advice.
CBT-I vs. Sleeping Pills: The Real Difference
Doctors still prescribe pills like zolpidem for insomnia. They work-for a while. But here’s what they don’t tell you: they don’t prevent depression from coming back.
A 2025 study in Nature Scientific Reports compared CBT-I and zolpidem. Both improved sleep and mood in the short term. But after six months, the CBT-I group stayed better. The zolpidem group? Their sleep and mood slipped back to where they started. Why? Pills don’t change your habits or beliefs. They just mask the problem.
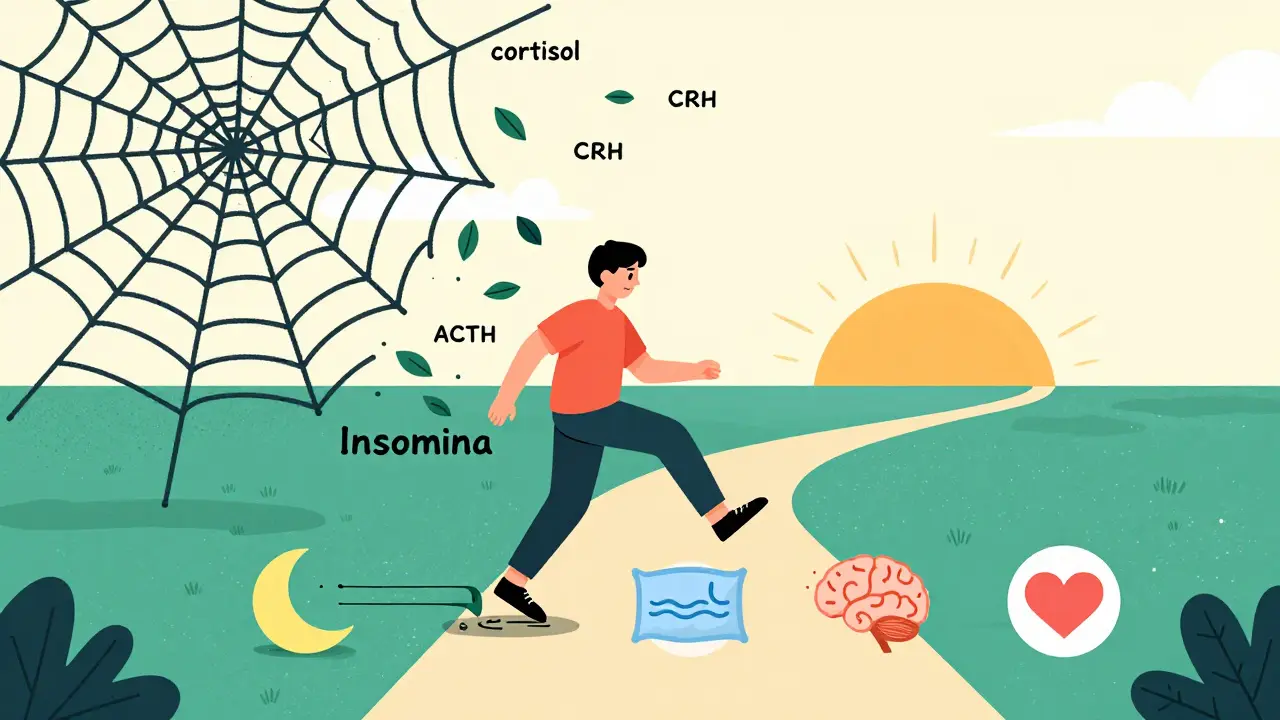
CBT-I works because it targets the biology behind the insomnia. People with depression and insomnia have overactive stress systems. Their bodies pump out too much cortisol, CRH, and ACTH-hormones that keep you alert. CBT-I brings those levels down. It’s not just psychological. It’s physiological.

Success Isn’t Just About Sleeping More
Not everyone who does CBT-I gets better. And not everyone who sleeps better gets less depressed. But here’s the key insight: remission of insomnia is what matters.
A 2023 review in Sleep journal found that people who fully recovered from insomnia (not just improved) had a 83% lower risk of developing major depression. Those who started CBT-I but didn’t fully recover? Their risk was still more than double that of good sleepers.
This means the goal isn’t to sleep 7 hours. It’s to stop the cycle of lying awake, stressing about it, and then feeling worse the next day. When insomnia lifts, depression and anxiety often follow-naturally.
Why So Few People Get CBT-I
Here’s the problem: CBT-I is hard to find. Only 1 to 2% of people with insomnia get it. In the U.S., fewer than 5% of psychologists are trained to deliver it. Insurance often won’t cover it. And even when it’s available, it takes time.
Many people give up because the first few weeks are tough. Sleep restriction means you’re tired. You might feel worse before you feel better. One study found 65 to 75% of patients feel worse during the first two weeks. But those who stick with it? 76% see clinically meaningful improvement in their sleep.
And the payoff? Treating insomnia cuts depression relapse risk by up to 50%. That’s bigger than any antidepressant alone. Kaiser Permanente started screening all depression patients for insomnia in 2022. Two years later, relapse rates dropped 22%.
What’s Next: Better Access, Better Results
The global insomnia treatment market is growing fast-projected to hit nearly $2 billion by 2030. Digital CBT-I platforms are leading the charge. With telehealth, you can start treatment from your couch. Some programs even sync with wearables to track sleep patterns.
New research is looking at combining CBT-I with antidepressants. A 2024 JAMA Psychiatry study found that patients taking sertraline plus CBT-I had 40% higher remission rates than those on the drug alone. For people who haven’t responded to medication, adding sleep therapy could be the breakthrough.
And the economics make sense. Every dollar spent on CBT-I returns $2.50 to $3.50 in reduced healthcare costs and better work performance. That’s not just good for you-it’s good for the system.
Where to Start
If you’re struggling with sleep and depression or anxiety, here’s what to do:
- Track your sleep for a week. Write down when you get in bed, when you fall asleep, when you wake up, and how you feel in the morning.
- Ask your doctor or therapist if they offer CBT-I. If not, ask for a referral.
- Look for digital programs like Sleepio, SHUTi, or CBT-I Coach. Many are covered by insurance now.
- Don’t give up if the first few weeks are hard. The discomfort is part of the fix.
- Remember: you’re not failing if you can’t sleep. You’re learning how to let sleep come back.
Insomnia and mental health aren’t separate problems. They’re two sides of the same coin. Fix one, and the other often follows. The science is clear. The tools exist. What’s missing is access-and the belief that sleep matters as much as mood.
Can insomnia cause depression, or is it just a symptom?
Insomnia isn’t just a symptom-it’s a known risk factor. Research shows people with chronic insomnia are 40 times more likely to develop major depression than those who sleep well. Treating insomnia can reduce the chance of depression developing in the first place, proving it’s not just a side effect but a driver.
Is CBT-I better than sleeping pills for depression-related insomnia?
Yes. While sleeping pills like zolpidem help you fall asleep faster, they don’t change the habits or thoughts keeping you awake. CBT-I addresses the root causes and leads to lasting improvements. Studies show CBT-I reduces depression relapse by up to 50%, while pills offer only short-term relief with no prevention benefit.
How long does CBT-I take to work?
Most people start seeing changes in 2 to 4 weeks, but full treatment usually takes 6 to 8 weeks. The first week can be tough-sleep restriction means less time in bed, which makes you tired. But by week 4, most report better sleep and less anxiety. The key is sticking with it, even when it feels hard.
Can I do CBT-I on my own with an app?
Yes. Digital CBT-I platforms like Sleepio and SHUTi have been clinically tested and shown to be as effective as in-person therapy. They guide you through the same steps-sleep restriction, stimulus control, cognitive restructuring-using videos, journals, and reminders. Many are covered by insurance and can be done from home.
What if CBT-I doesn’t work for me?
About 30 to 40% of people don’t fully recover from insomnia with CBT-I alone. That doesn’t mean it failed-it means you might need a different approach. Some people benefit from combining CBT-I with antidepressants. Others need more support for anxiety or trauma. Talk to your provider about adjusting your plan. The goal is not perfection-it’s progress.
Why isn’t CBT-I more widely available?
Fewer than 5% of U.S. psychologists are trained in CBT-I, and insurance often doesn’t cover it. Training takes time, and many providers still default to prescribing pills. But demand is rising. Telehealth and digital platforms are helping close the gap. If you can’t find a specialist, look for a digital program-they’re proven, accessible, and often covered.

Mark Able
December 17, 2025 AT 17:30Bro I tried CBT-I for 3 weeks and honestly thought I was gonna lose my mind. Sleep restriction had me napping at my desk like a zombie. But then-week 4-I slept 7 hours straight for the first time in 2 years. No pills. No magic. Just dumb consistency. Now I actually wake up excited instead of dreading the day. If you’re on the fence, just start the damn app. You’ll thank yourself later.
Dorine Anthony
December 19, 2025 AT 08:09Just wanted to say thank you for posting this. I’ve been struggling for years and felt so alone. The part about insomnia being a driver, not just a symptom, made me cry. I didn’t realize I wasn’t broken-I was just stuck in a loop. CBT-I feels scary but now I think it’s my best shot.
William Storrs
December 19, 2025 AT 16:16Look, I get it. It’s hard. The first two weeks feel like punishment. But here’s the truth: your brain is rewiring. You’re not failing-you’re healing. I’ve coached 12 people through this. Every single one who stuck with it said the same thing: ‘I wish I’d started sooner.’ Don’t quit because it’s uncomfortable. Quit because you’re better. And you will be.
James Stearns
December 20, 2025 AT 12:36While I commend the author for attempting to disseminate rudimentary clinical insights, one must acknowledge the profound epistemological limitations inherent in contemporary behavioral paradigms. The conflation of symptom and etiology, while clinically convenient, fails to account for the neuroendocrinological cascade precipitated by circadian dysregulation. Furthermore, the commodification of CBT-I via digital platforms represents a troubling regression toward algorithmic paternalism, wherein human agency is subsumed by corporate wellness ecosystems masquerading as therapeutic innovation.
Nina Stacey
December 21, 2025 AT 14:11OMG I just started sleepio last week and it’s wild like I used to think I needed 8 hours and now I’m like okay maybe 5 is fine if I’m not falling asleep in 20 minutes I just get up and drink tea and read and it’s not the end of the world and I feel way less panicked about it honestly I never thought I’d say this but I think I’m starting to like my brain again
Dominic Suyo
December 22, 2025 AT 10:41CBT-I? More like CBT-I’m-Tired-Of-This. Let’s be real-sleep apps are just corporate snake oil wrapped in peer-reviewed jargon. Meanwhile, the real problem is our culture’s obsession with productivity. We’re not broken-we’re exhausted. You don’t need to ‘rewire’ your brain. You need to stop being a cog in a machine that doesn’t care if you sleep. Sleep restriction? More like soul restriction.
Kevin Motta Top
December 22, 2025 AT 15:44My dad had insomnia for 15 years. Tried everything. Then did CBT-I via telehealth. Slept like a baby after 6 weeks. Now he’s hiking, cooking, laughing again. It’s not hype. It’s science with legs.
Alisa Silvia Bila
December 24, 2025 AT 14:17I was skeptical but tried SHUTi after my therapist pushed me. The first week was brutal-I felt worse. But by week 5, I noticed I wasn’t checking the clock at 3am anymore. That was the turning point. It’s not about sleeping more. It’s about stopping the panic. That’s what changed everything.
William Liu
December 26, 2025 AT 10:06Just finished my 8-week CBT-I course. I didn’t just sleep better-I stopped having panic attacks before bed. This isn’t just a sleep fix. It’s a mental health reset. If you’re reading this and you’re tired of being tired, do it. No excuses.
Aadil Munshi
December 26, 2025 AT 17:41Interesting how the West treats sleep like a problem to be optimized rather than a sacred rhythm to be honored. In my village in India, we didn’t have apps or sleep trackers-we had moonlight, silence, and the understanding that rest isn’t a performance. Still, I’m glad you’re finding tools that work. Just don’t let technology replace the soul of rest.
Frank Drewery
December 27, 2025 AT 02:23I’ve been in therapy for depression for 3 years. Nothing stuck. Then my therapist asked about my sleep. I laughed. She said, ‘Let’s try CBT-I.’ Six weeks later, I cried for the first time in months-not from sadness, but relief. This isn’t a side note. It’s the foundation.