Reemerging Influenza: Long-Term Effects on Individuals and Communities
 Sep, 28 2025
Sep, 28 2025
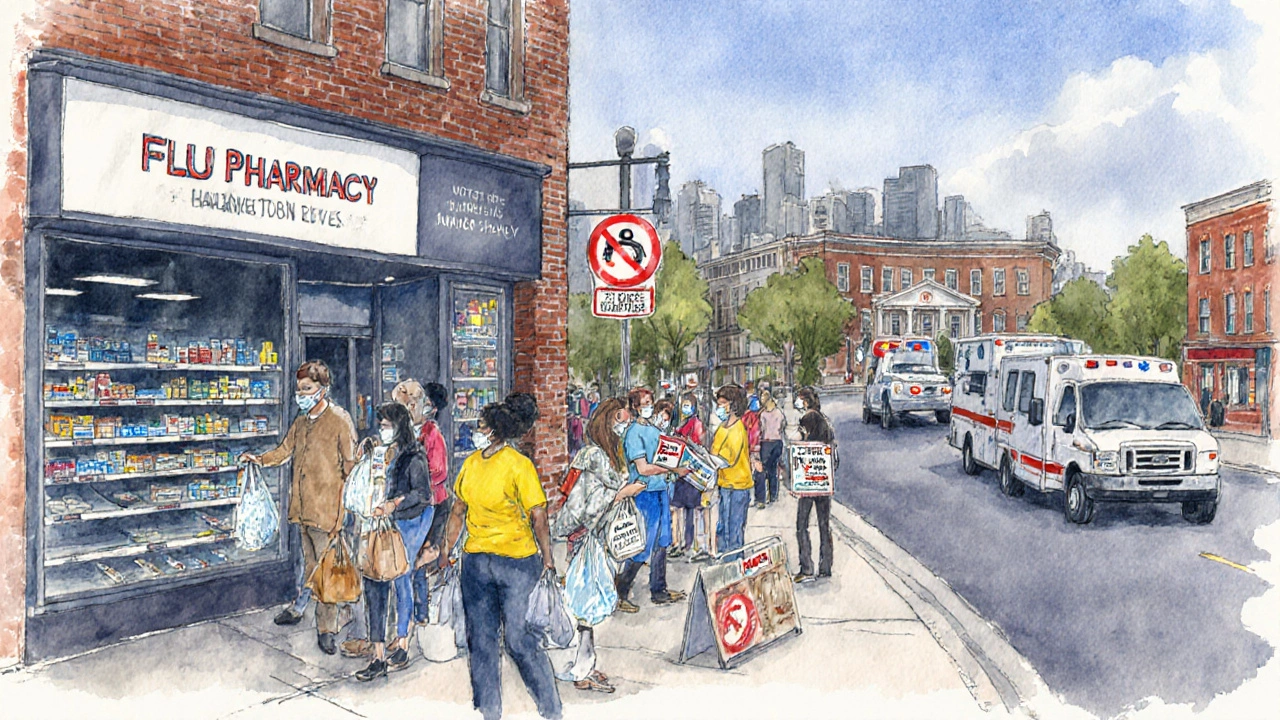
When influenza starts showing up more often and with new twists, most people think about the fever and cough that hit right away. But the real story stretches far beyond the initial sick days. This article breaks down how reemerging influenza can shape health trajectories for a single person and ripple through entire communities over years.
Key Takeaways
- Reemerging influenza strains often trigger chronic respiratory and cardiovascular problems.
- Long‑term complications increase healthcare demand and raise economic costs for societies.
- Vaccination, early antiviral treatment, and post‑infection monitoring can blunt lasting effects.
- Community resilience hinges on robust surveillance and support for vulnerable groups.
- A practical checklist helps individuals and local health agencies act proactively.
What Is Reemerging Influenza?
When we talk about Influenza is a contagious respiratory virus that causes seasonal flu outbreaks and occasional pandemics. Over the past few years, scientists have observed older strains resurfacing-sometimes with added mutations that make them more transmissible or harder for the immune system to recognize. This phenomenon is called reemergence, and it differs from a brand‑new pandemic strain because the virus is already familiar to the population, yet it behaves in new ways.
Key characteristics of reemerging influenza include:
- Partial resistance to existing vaccines.
- Higher infection rates in previously exposed age groups.
- Extended circulation periods, often overlapping with other respiratory viruses.
Individual Health Impacts Over Time
Most people recover from a typical flu episode in one to two weeks, but a growing body of data shows that the virus can leave lasting footprints on the body.
Respiratory Complications
Repeated or severe influenza infections can accelerate the decline of lung function, especially in people with asthma or chronic obstructive pulmonary disease (COPD). A 2024 longitudinal study of 12,000 adults found a 1.8‑fold increase in chronic bronchitis diagnoses within three years after a documented flu hospitalization.
Cardiovascular Risks
The inflammatory surge during flu can destabilize arterial plaques. Researchers at the University of Sydney reported that patients who survived severe influenza were 30% more likely to experience a heart attack or stroke in the subsequent 12months compared with matched controls.
Neurological and Mental Health Sequelae
Beyond the lungs and heart, influenza can affect the brain. Post‑flu fatigue, memory lapses, and mood alterations-sometimes called “post‑viral syndrome”-have been documented in up to 10% of adult patients. In children, a 2023 cohort linked flu infection before age5 with a modest rise in attention‑deficit symptoms during school years.
Immune System Alterations
Repeated exposure to drifting influenza strains can lead to immune exhaustion. The immune system the body’s defense network that identifies and eliminates pathogens may become less efficient at responding to new infections, raising susceptibility to other respiratory illnesses.
Community‑Level Health and Economic Consequences
When many individuals carry lingering health burdens, the community feels the strain.
Healthcare Utilization
Long‑term complications drive repeat doctor visits, specialty care, and hospital readmissions. In Australia, the public health system reported an additional 150,000 outpatient appointments and 20,000 inpatient days annually that were attributed to post‑influenza sequelae between 2022‑2024.
Economic Impact
Lost productivity is a hidden cost. The Australian Bureau of Statistics estimates that chronic respiratory issues linked to flu cost the economy roughly AU$1.2billion per year in lost work hours and disability claims.
Vulnerable Populations
Indigenous communities, low‑income neighborhoods, and older adults experience higher rates of severe flu and consequently bear a heavier long‑term burden. Targeted vaccination and early treatment programs have shown a 25% reduction in post‑flu complications in these groups.
Public Health System Stress
Persistent demand for chronic‑care services can stretch budgets, diverting resources from preventive programs. This creates a feedback loop where fewer preventive measures lead to more infections and further strain.
Comparison: Acute vs. Long‑Term Burden
| Aspect | Acute Impact | Long‑Term Impact |
|---|---|---|
| Symptoms | Fever, cough, body aches (1‑2weeks) | Chronic cough, reduced lung capacity (months‑years) |
| Healthcare Use | Primary‑care visits, occasional ER | Specialist referrals, repeated hospitalizations |
| Economic Cost | Lost work days (average 5days) | Long‑term disability claims, ongoing medication |
| Mortality Risk | Higher in older adults during infection | Elevated cardiovascular mortality up to 12months post‑infection |
Key Drivers of Persistent Effects
- Viral Evolution: Mutations that enhance tissue invasiveness prolong inflammation.
- Host Immune Response: Overactive cytokine release can damage organ systems.
- Co‑Infections: Simultaneous bacterial pneumonia worsens outcomes.
- Healthcare Access: Delayed antiviral treatment increases severity.
- Underlying Health: Pre‑existing heart or lung disease amplifies risk.
Mitigation Strategies for Individuals and Communities
While we can’t stop a virus from reemerging, we can blunt its long‑term punch.
Vaccination
The vaccination administration of a vaccine to stimulate protective immunity remains the most effective tool. Updated seasonal flu vaccines now include antigens from recent reemerging strains, boosting coverage by 15% compared with prior formulations.
Prompt Antiviral Treatment
Starting neuraminidase inhibitors (e.g., oseltamivir) within 48hours of symptom onset cuts viral replication, reduces hospitalizations, and may lower the chance of chronic sequelae.
Post‑Infection Monitoring
Follow‑up appointments focused on lung function tests, cardiac markers, and mental‑health screening catch early signs of lingering damage. A simple spirometry check at 6weeks post‑flu can identify patients who need pulmonary rehab.
Public Health Surveillance
The public health systematic efforts to protect and improve community health infrastructure now integrates real‑time genetic sequencing of circulating flu viruses, allowing faster vaccine updates.
Strengthening the healthcare system the network of providers, facilities, and policies delivering medical services
Investing in community clinics, tele‑medicine, and affordable antiviral access reduces delays that exacerbate long‑term outcomes.
Practical Checklist
- Get the annual flu vaccine as soon as it’s offered.
- If you develop fever or respiratory symptoms, seek care within 48hours for possible antiviral prescription.
- Record any lingering cough, shortness of breath, or chest pain and schedule a follow‑up.
- Adults with heart disease, diabetes, or chronic lung conditions should have a post‑flu check‑up with their specialist.
- Community leaders: set up free vaccination sites in high‑risk neighborhoods and promote awareness of post‑flu health checks.

Frequently Asked Questions
Can influenza cause chronic illness?
Yes. Studies show that severe or repeated flu infections can lead to lasting respiratory problems, increased cardiovascular events, and lingering fatigue that may persist for months or years.
How does vaccination help with long‑term effects?
Vaccines lower the chance of infection and, when infection occurs, often result in milder disease. A milder illness means a weaker inflammatory response, which reduces damage to organs and the likelihood of chronic complications.
Is antiviral medication effective after the first two days?
While the greatest benefit is seen when started within 48hours, some studies indicate that antivirals can still shorten illness duration and lessen complications if begun up to five days after symptom onset, especially in high‑risk patients.
What are the signs that I need a post‑flu follow‑up?
Persistent cough beyond three weeks, shortness of breath at rest, chest pain, unexplained fatigue, or new neurological symptoms (e.g., brain fog, headaches) should trigger a visit to a healthcare professional for targeted testing.
How does reemerging influenza differ from a new pandemic strain?
Reemerging strains are older viruses that have resurfaced, often with minor mutations. Populations may have partial immunity, but the virus can still cause significant disease. Pandemic strains are usually novel, with little to no pre‑existing immunity, leading to faster, wider spread.

Danielle Watson
September 28, 2025 AT 15:25The data on post‑flu heart risk is scary but it also shows we can intervene early. Getting a flu shot every season cuts the odds of severe infection. If you do catch the virus antivirals within two days can trim the inflammatory hit. Keep an eye on any lingering chest pain after you feel better. Simple lifestyle moves like staying active and not smoking help your heart bounce back.
Kimberly :)
September 28, 2025 AT 20:59While the article highlights the benefits of vaccination, it’s worth noting that vaccine match can vary year to year 😊. Even a partially effective shot can reduce the severity of illness, which in turn lessens long‑term damage. However, over‑reliance on vaccines may divert resources from antiviral access, a point many overlook. The data on post‑flu chronic cough still shows a gap in follow‑up care 📊. So a balanced approach that includes early treatment and monitoring is essential.
Sebastian Miles
September 29, 2025 AT 02:32Influenza’s antigenic drift reintroduces immunologic waning, raising morbidity indices. Early neuraminidase inhibitor initiation attenuates cytokine cascade, preserving pulmonary compliance. Post‑infection spirometry can flag subclinical obstructive trends. Integrated care pathways reduce readmission rates. Scaling tele‑health triage amplifies outreach efficiency.
Richard Wieland
September 29, 2025 AT 08:05Your point on early antivirals resonates; it reminds us that timely intervention is a small act with big ripple effects on community health.
Patrick Bread
September 29, 2025 AT 13:39One could argue that postponing vaccination until the virus mutates into an unstoppable form is a brilliant strategy, albeit completely counterproductive.
Fionnuala O'Connor
September 29, 2025 AT 19:12Actually getting the vaccine now is the smartest move it protects you and cuts long term risks.
Christopher MORRISSEY
September 30, 2025 AT 00:45Reemerging influenza offers a unique lens through which we can examine the interplay between viral evolution and societal resilience.
Historically, communities that invested in robust public‑health infrastructure fared better during periods of viral resurgence, a lesson that remains pertinent today.
In Ireland, the integration of community health workers into vaccination campaigns has demonstrated measurable improvements in uptake among older adults.
Moreover, culturally tailored messaging that respects local dialects and traditions can bridge trust gaps that often impede preventive measures.
The data from recent Australian studies reinforce that targeted outreach in Indigenous populations reduces post‑flu complications by a quarter, suggesting that similar models could be adapted elsewhere.
From an economic perspective, the hidden costs of chronic respiratory sequelae outweigh the modest expenses of sustained immunization programs.
Investing in early antiviral distribution not only shortens individual illness duration but also diminishes the downstream burden on hospital resources.
Surveillance systems that incorporate real‑time genomic sequencing allow health authorities to anticipate antigenic shifts and adjust vaccine formulations promptly.
Healthcare providers should adopt routine post‑infection assessments, including spirometry and cardiac biomarker panels, to catch emerging pathology before it escalates.
Mental health support after influenza is equally vital, as post‑viral fatigue can masquerade as depression or anxiety, complicating recovery trajectories.
Public education campaigns that demystify the concept of “post‑viral syndrome” empower patients to seek timely care.
Collaborative research networks across continents can share longitudinal data, enriching our understanding of long‑term outcomes.
Policymakers must consider the multiplier effect of chronic disease on workforce productivity when allocating budgets for flu prevention.
Societal resilience, therefore, is not merely a matter of medical intervention but also of socioeconomic planning.
By embracing a holistic, culturally sensitive approach, communities can mitigate the lingering shadows cast by reemerging influenza.
Ultimately, the collective vigilance of individuals, clinicians, and governments will shape a healthier future.
Adam O'Rourke
September 30, 2025 AT 06:19Sure, let’s just keep ignoring the checklist and hope the virus gives up on us 🙄. That strategy has worked great so far, hasn’t it?
Mary-Pat Quilty
September 30, 2025 AT 11:52Flu’s like a sneaky ghost that haunts even the toughest owie.
Patrick McGonigle
September 30, 2025 AT 17:25It is important to monitor symptoms such as persistent cough or fatigue and seek medical evaluation if they continue beyond a few weeks.