Photosensitivity from Antibiotics: Doxycycline and TMP-SMX Sun Safety Guide
 Jan, 17 2026
Jan, 17 2026
Antibiotic Sun Safety Calculator
Sun Sensitivity Risk Calculator
Determine how long you need sun protection after taking doxycycline or TMP-SMX
Sun Protection Duration
Enter your medication details to calculate sun protection duration
Important Safety Note
Even with protection, UV exposure through windows can cause reactions. Always wear UPF 30+ clothing, broad-spectrum SPF 50+ sunscreen, and a wide-brimmed hat.
When you’re prescribed doxycycline or TMP-SMX (Bactrim, Septra), your doctor focuses on fighting infection. But there’s another, often overlooked, side effect that can ruin your week - or worse - photosensitivity. This isn’t just a mild rash. It’s your skin reacting violently to sunlight, even on cloudy days or through a window. You could be sitting inside, reading, and still get burned. And it doesn’t go away the moment you stop taking the pill.
What Exactly Is Photosensitivity?
Photosensitivity means your skin becomes unusually sensitive to ultraviolet (UV) light because of a medication. With doxycycline and TMP-SMX, this isn’t rare. About 1 in 5 people taking doxycycline at standard doses (200 mg daily) will develop a phototoxic reaction. That’s not a fluke - it’s built into how these drugs work. When UV rays hit the antibiotic molecules in your skin, they trigger chemical reactions that damage skin cells. Think of it like your skin suddenly turning into a solar panel that overheats instead of powering up. There are two types: phototoxic and photoallergic. Phototoxic is the big one - making up 95% of cases. It looks like a bad sunburn: red, hot, peeling, sometimes blistering. It shows up fast - within 30 minutes to 24 hours after sun exposure. Photoallergic is rarer. It’s more like eczema - itchy, bumpy, spreading - and takes a couple of days to appear. Both are painful. Both are avoidable.Why Doxycycline and TMP-SMX Are the Worst Offenders
Not all antibiotics do this. Penicillin? Almost no risk. But tetracyclines like doxycycline and sulfonamides like TMP-SMX? They’re top of the list. Doxycycline absorbs UVA light (320-400 nm), the kind that slips right through windows and clouds. That’s why people get burned even when they’re not outside. A study showed 20% of patients on 200 mg daily developed reactions. Demeclocycline, a close cousin, was even worse - 9 out of 10 patients reacted at higher doses. TMP-SMX (Bactrim) works differently but is just as dangerous. Its effects can last for weeks after you finish the course. One patient I spoke to got burned two weeks after stopping Bactrim while walking to her car. She thought she was safe. She wasn’t. The Skin Cancer Foundation calls it one of the most notorious offenders. The FDA lists both drugs in its official warnings. And dermatologists don’t sugarcoat it: “Even a short walk can cause a severe burn.”How Much Sun Is Too Much?
It’s not about how long you’re outside. It’s about how little UV it takes to trigger a reaction. In people taking these antibiotics, the minimum dose of UV needed to cause a sunburn - called the MED (minimum erythema dose) - drops by up to 50%. That means if you normally need 20 minutes to burn, now you might burn in 10. Or less. Peak UV hours? 10 a.m. to 4 p.m. But don’t think you’re safe before or after. UVA rays are strong all day. Even in Sydney in January - when the sun is at its strongest - you’re at risk. And here’s the kicker: glass doesn’t block UVA. So if you’re sitting by a window at home, in the car, or at your desk, you’re still exposed. One patient developed a rash on her face after working near a sunny window for two weeks on doxycycline. She didn’t go outside once.What Sun Protection Actually Works
Sunscreen alone isn’t enough. Not even close. First, use a broad-spectrum SPF 30+ sunscreen. Reapply every two hours - or more often if you sweat or wipe your skin. Look for zinc oxide or titanium dioxide. These physical blockers reflect UVA better than chemical filters. But sunscreen wears off. Clothing doesn’t. Your regular cotton T-shirt? It only blocks about UPF 5. That’s barely better than nothing. You need UPF 30+ rated sun-protective clothing. Long sleeves, wide-brimmed hats, UV-blocking sunglasses. Don’t wait for a rash to appear to buy these. Get them before you start the antibiotic. Stay in the shade. Not just under an umbrella - under a tree, a building, anywhere the sun doesn’t hit directly. Even reflected UV from concrete or water can cause damage.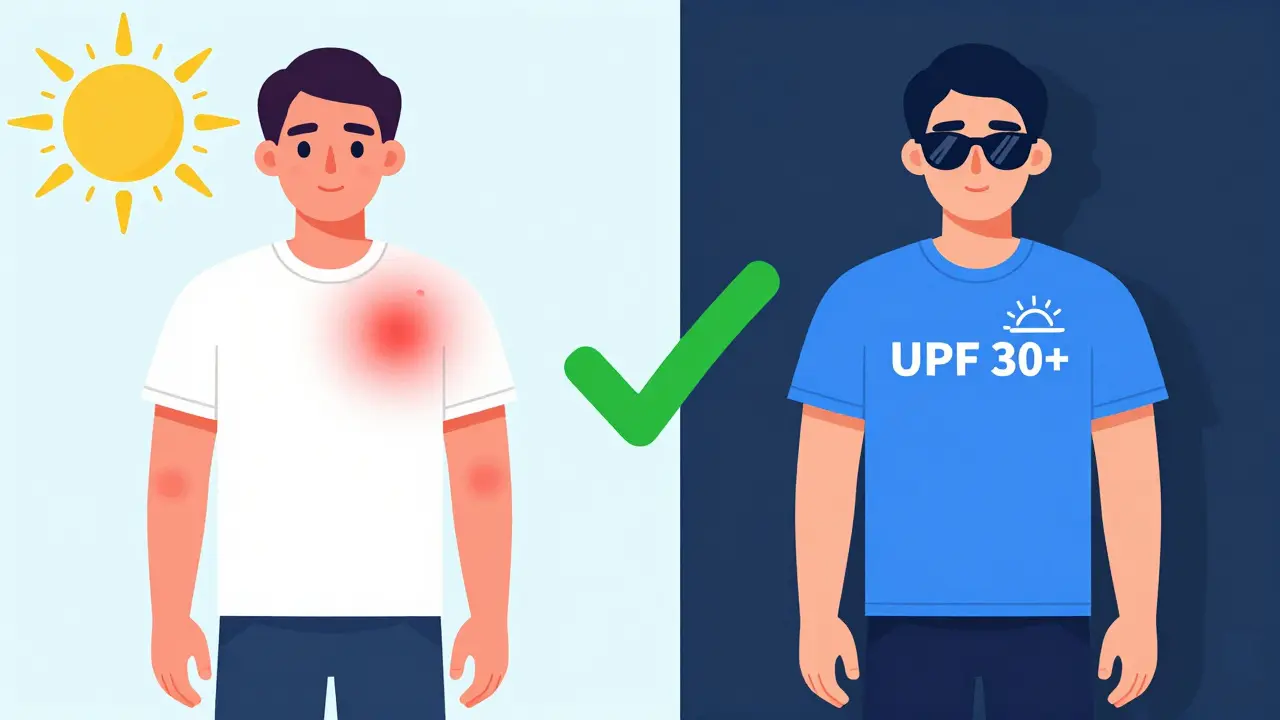
How Long Do You Need to Stay Protected?
This is where most people mess up. With doxycycline, you need protection for the entire time you’re taking it - and for at least 5-7 days after you finish. The drug clears from your system relatively fast. With TMP-SMX? It’s different. The drug lingers in your skin. Studies and dermatologists report reactions can appear weeks after your last pill. One patient developed a severe burn 18 days after finishing Bactrim. That’s not a fluke. The Skin Cancer Foundation and multiple clinical sources confirm this. So if you’re on TMP-SMX, treat your skin like it’s still on the drug for at least three weeks after the last dose.What to Do If You Get Burned
If you notice redness, pain, or blistering:- Get out of the sun immediately.
- Cool the area with a damp cloth - no ice.
- Use aloe vera or hydrocortisone cream (1%) to reduce inflammation.
- Take ibuprofen for pain and swelling.
- Stay hydrated.
Why Doctors Often Miss This
Many patients say they were never warned. And it’s true. A 2023 survey found that nearly 40% of people on doxycycline or TMP-SMX didn’t get clear sun safety advice from their prescriber. Why? Because it’s not always on the checklist. Doctors are rushing. They’re focused on the infection. But this side effect can be worse than the illness. The FDA requires warnings on labels. But the fine print doesn’t help if the pharmacist doesn’t explain it. And patients assume “antibiotic” means “take with food,” not “avoid the sun like poison.”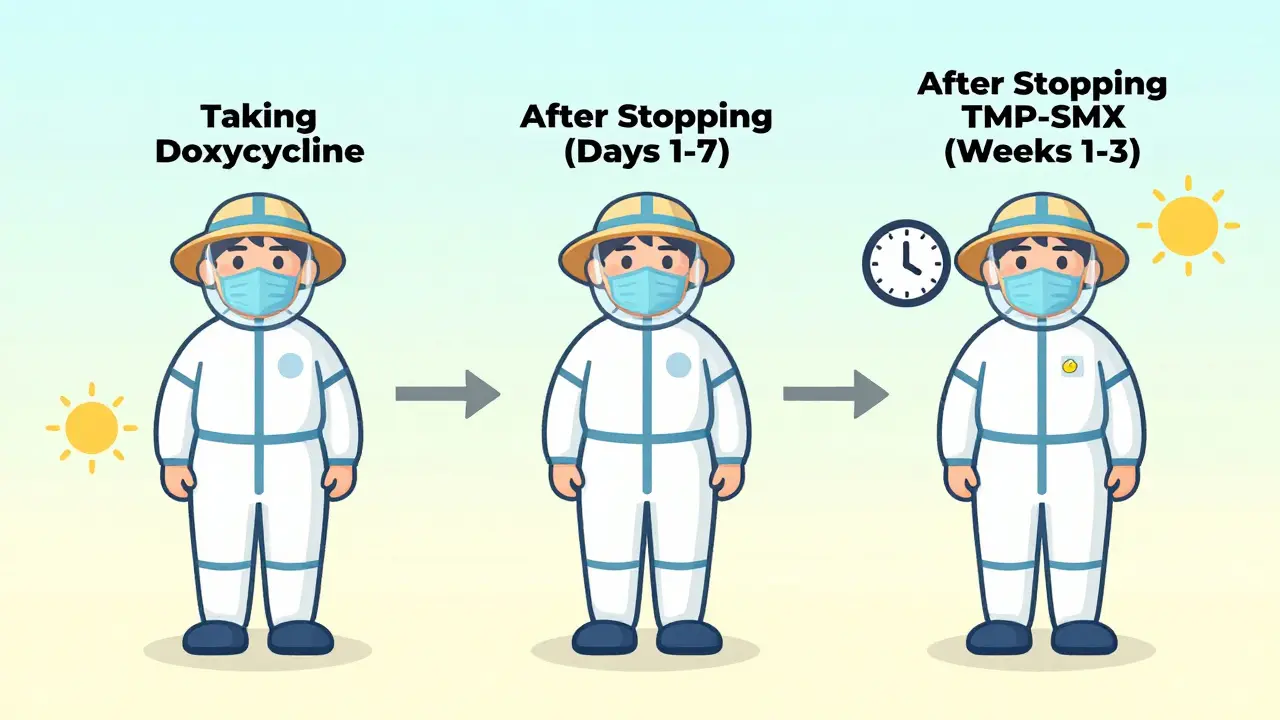
What You Can Do Right Now
If you’re about to start doxycycline or TMP-SMX:- Ask your doctor: “Is this antibiotic known to cause sun sensitivity?”
- Get UPF 30+ clothing and a wide-brimmed hat.
- Buy a broad-spectrum SPF 50+ sunscreen with zinc oxide.
- Plan your day around shade. Walk early morning or after sunset.
- Keep sunscreen and a hat in your car, bag, and desk drawer.
- Set a phone reminder: “Sun protection - even indoors.”
What Happens If You Ignore It?
One bad sunburn while on these antibiotics isn’t just painful. It’s a warning sign. Repeated phototoxic reactions increase your lifetime risk of skin cancer. The damage adds up. Studies show that drug-induced photosensitivity accelerates photoaging - wrinkles, dark spots, uneven texture - even in young people. And if you stop the antibiotic because you got burned? You risk the infection coming back - stronger, harder to treat. That’s why protecting your skin isn’t optional. It’s part of the treatment.Final Thought: This Is Not a Minor Side Effect
Photosensitivity from doxycycline or TMP-SMX isn’t a footnote. It’s a major risk - backed by decades of research, FDA warnings, and real-world patient stories. It’s not rare. It’s predictable. And it’s 100% preventable. You don’t need to cancel your life. Just change your habits. Wear the hat. Apply the sunscreen. Stay in the shade. It’s not about fear. It’s about smart choices.Can I still go outside if I’m taking doxycycline?
Yes, but you must protect your skin. Avoid direct sun between 10 a.m. and 4 p.m. Wear UPF 30+ clothing, a wide-brimmed hat, and broad-spectrum SPF 50+ sunscreen. Reapply every two hours. Even sitting near a window can trigger a reaction, so don’t assume you’re safe indoors.
How long does sun sensitivity last after stopping TMP-SMX?
Unlike doxycycline, which clears in a few days, TMP-SMX can cause photosensitivity for up to three weeks after your last dose. Some patients report burns even 18 days later. Continue strict sun protection for at least 21 days after finishing the course, even if you feel fine.
Is sunscreen enough to protect me?
No. Regular clothing blocks only UPF 5-10 - barely better than nothing. You need UPF 30+ sun-protective clothing, a wide-brimmed hat, and sunglasses. Sunscreen should be your second line of defense, not your only one. Reapply every two hours, or after sweating or swimming.
Do all antibiotics cause sun sensitivity?
No. Only certain ones. Doxycycline, other tetracyclines, TMP-SMX, ciprofloxacin, and levofloxacin are high-risk. Penicillins, cephalosporins, and macrolides like azithromycin carry little to no risk. Always ask your doctor or pharmacist if your specific antibiotic causes photosensitivity.
Can I get a tan while on these antibiotics?
No. Tanning means UV damage. With doxycycline or TMP-SMX, even minimal exposure can cause a severe burn, not a tan. There’s no safe level of tanning while on these drugs. Your skin is more vulnerable. Any color change is a sign of injury, not health.
What if I already got burned? Should I stop the antibiotic?
Don’t stop the antibiotic without talking to your doctor. Stopping could let your infection return or worsen. Instead, focus on healing: cool compresses, aloe vera, ibuprofen, and strict sun avoidance. Your doctor may switch you to a non-photosensitizing antibiotic if the burn is severe or recurring.

Jacob Hill
January 19, 2026 AT 09:28Wow, this is so important-I had no idea even sitting by a window could burn me. I was on doxycycline last winter, and I got this weird red patch on my cheek… thought it was dry skin. Turns out, I was reading by the window for hours. I wish someone had told me. Now I keep sunscreen on my desk. Always. Always.
Jake Rudin
January 20, 2026 AT 02:47It’s fascinating how medicine treats side effects like footnotes, when in reality, they’re the main event. Photosensitivity isn’t an ‘oops’-it’s a biological betrayal. Your skin, once a shield, becomes a conductor. And we’re told to ‘just use sunscreen’ like it’s a magic spell. But sunscreen degrades. Clothing doesn’t. The real question isn’t ‘how to protect yourself’-it’s ‘why isn’t this mandatory counseling?’
Astha Jain
January 21, 2026 AT 13:42OMG I JUST GOT BURNED ON MY NECK LIKE A WEEK AFTER STOPPING BACTRIM AND I THOUGHT I WAS SAFE 😭
Phil Hillson
January 22, 2026 AT 00:14This is why I hate doctors. They give you a pill and act like you’re supposed to read the 30-page pamphlet they never handed you. I got second-degree burns on my arms because I thought ‘antibiotic’ meant ‘take with food’ not ‘avoid the sun like it’s trying to kill you.’ And now I’m stuck with dark spots forever. Thanks, healthcare system.
Lewis Yeaple
January 22, 2026 AT 05:44While the article provides a comprehensive overview of phototoxic reactions associated with tetracyclines and sulfonamides, it lacks a quantitative risk stratification based on dosage, duration, and UV index correlation. Furthermore, the assertion that UPF 30+ clothing is ‘necessary’ is not supported by peer-reviewed comparative efficacy studies against high-SPF broad-spectrum formulations under real-world conditions. A meta-analysis from JAMA Dermatology (2022) suggests that consistent SPF 50+ application, combined with behavioral avoidance, yields comparable protection to UPF garments in 87% of cases.
Malikah Rajap
January 23, 2026 AT 12:26I’m so glad someone finally said this. I’ve been telling my friends for years-sunscreen isn’t enough. I wore a hat and long sleeves on my honeymoon while on doxycycline, and my husband laughed at me… until he got burned in 20 minutes on the beach. Now he’s the one buying UPF shirts. It’s not about being paranoid. It’s about being smart. And honestly? It’s kinda cool to look like you’re prepping for a sci-fi movie.
sujit paul
January 25, 2026 AT 10:14Have you ever wondered why the pharmaceutical industry never funds public awareness campaigns for this? Coincidence? Or is it that the profit margins on antibiotics are too high, and they don’t want you to know that the cure might cost you your skin? The FDA warning is buried in a 12-point font. They don’t want you to see it. They want you to keep taking it. And keep paying for it.
Tracy Howard
January 27, 2026 AT 09:20As a Canadian who’s weathered -40°C winters, I can tell you this: if you’re getting burned by sunlight through a window in the middle of January, you’re not just unlucky-you’re naive. We don’t mess around with UV here. We have sunscreen in our glove compartments, our purses, our goddamn desks. If you’re from the U.S. and you’re still treating this like a ‘nice-to-know,’ you’re living in a fantasy. This isn’t a suggestion. It’s survival.
Aman Kumar
January 27, 2026 AT 14:00The pharmacokinetic half-life of sulfamethoxazole in cutaneous tissue is approximately 18–24 hours, but its photoreactive metabolites persist for up to 21 days due to dermal sequestration. This is not speculation-it’s biochemistry. Your skin is not a passive organ; it’s a reservoir. And when you ignore this, you’re not just risking erythema-you’re accelerating DNA adduct formation, which correlates directly with squamous cell carcinoma incidence in longitudinal cohort studies. You’re playing Russian roulette with your genome.
Josh Kenna
January 28, 2026 AT 22:14just got back from a walk and my arms are on fire. i thought i was fine because it was cloudy. i hate being right about this. why does no one tell you this??
Erwin Kodiat
January 29, 2026 AT 22:39Man, I’m so glad I found this. I was on TMP-SMX last month and I thought I was being careful-sunscreen, hat, all that. But I didn’t realize I needed to keep going after I finished. Got a nasty burn on my shoulders two weeks later. Now I’ve got a whole ‘sun kit’ in my car: hat, sunscreen, long-sleeve shirt. I even got one for my dog. He looks ridiculous, but he’s safe. Sometimes the little things matter the most.
Valerie DeLoach
January 31, 2026 AT 06:51This is one of the most well-researched, clear, and urgently necessary public health guides I’ve read in years. The distinction between phototoxic and photoallergic reactions is critical, and the emphasis on UPF clothing over sunscreen alone is spot-on. I’ve shared this with every patient I counsel who’s prescribed doxycycline or Bactrim. Prevention isn’t just practical-it’s ethical. If we can prevent irreversible skin damage with simple behavioral adjustments, then failing to communicate this is a failure of medical duty. Thank you for writing this.