How the FDA Ensures Generic Drugs Work the Same as Brand-Name Medications
 Nov, 26 2025
Nov, 26 2025
When you pick up a prescription at the pharmacy, there’s a good chance it’s a generic drug. About 90% of all prescriptions filled in the U.S. are generics. That’s not because doctors are cutting corners-it’s because the FDA has made sure these drugs work just like the brand-name versions, at a fraction of the cost. But how do they know? What’s really going on behind the scenes to guarantee that a $5 generic pill does the same job as a $50 brand-name one?
The FDA’s Hidden Science: Bioequivalence
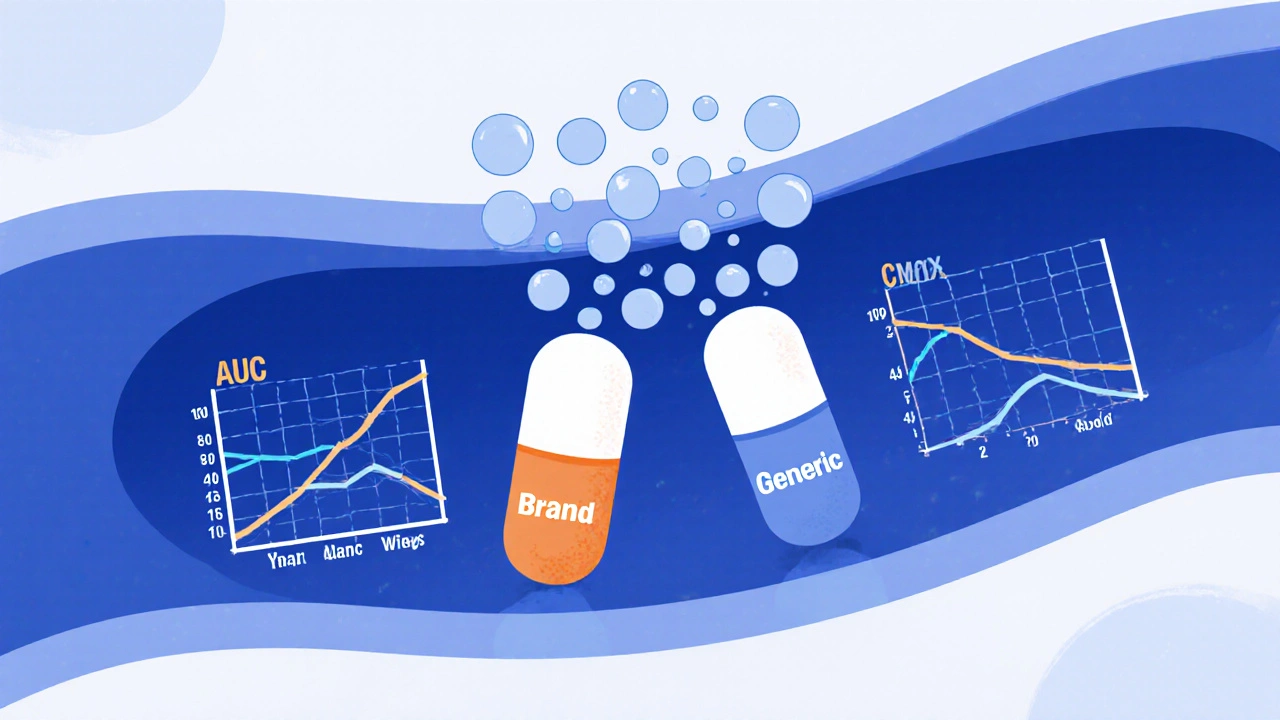
The core of the FDA’s approval process for generics is something called bioequivalence. It sounds technical, but it’s simple in practice: the generic drug must get into your bloodstream at the same rate and in the same amount as the brand-name drug. Not close. Not almost. Exactly within a narrow, scientifically proven range.To prove this, manufacturers run clinical studies-usually with 24 to 36 healthy volunteers. These people take the brand-name drug on one day, then the generic on another, with a clean break in between. Blood samples are taken over several hours to measure how much of the active ingredient enters the bloodstream and how fast. The results are compared using two key numbers: AUC (area under the curve, which shows total exposure) and Cmax (the peak concentration).
The FDA requires that the generic’s AUC and Cmax fall within 80% to 125% of the brand-name drug’s values. That’s not a guess. It’s a legally binding standard written into 21 CFR Part 320. The 90% confidence interval for both numbers must land inside that range. If it doesn’t, the application gets rejected. No exceptions.
This isn’t theoretical. For example, if a brand-name drug delivers 100 units of active ingredient into the blood, the generic must deliver between 80 and 125 units. That’s tight enough to ensure consistent effects-especially for drugs where small changes can matter, like blood thinners or thyroid meds.
More Than Just the Active Ingredient
It’s not enough for the generic to have the same active ingredient. It must also match the brand in strength, dosage form, and how it’s taken. A 10mg tablet of the brand must be a 10mg tablet in the generic. A capsule can’t be swapped for a liquid unless the label says it’s an alternative form. The route of administration-oral, injectable, topical-must be identical.Inactive ingredients? Those can be different. The generic might use a different filler, dye, or coating. But the FDA doesn’t just accept any additive. Every excipient must be listed in the agency’s Inactive Ingredient Database, which sets safe concentration limits for over 500 substances across 80 delivery methods. If a manufacturer wants to use something new, they have to prove it won’t affect how the drug is absorbed or cause side effects.
Even the size and shape of a pill matters-not for effectiveness, but for consistency. The FDA requires content uniformity testing: each tablet in a batch must contain between 85% and 115% of the labeled amount of active ingredient. That’s stricter than many food quality standards.
The ANDA Process: Fast, But Not Easy
Generic manufacturers don’t have to repeat the 10-year, billion-dollar clinical trials that brand-name companies run. Instead, they file an Abbreviated New Drug Application, or ANDA. The name says it all: abbreviated. But don’t let that fool you. An ANDA isn’t a shortcut-it’s a deep dive into science and manufacturing.Each ANDA submission runs between 30,000 and 50,000 pages. That’s the equivalent of a small encyclopedia. The bioequivalence section alone can be 5,000 to 10,000 pages of raw data, statistical models, and lab reports. The FDA reviews every page. In 2022, they approved 777 ANDAs. But nearly 35% of initial submissions were refused outright because of missing or flawed information.
Common reasons for rejection? Inadequate bioequivalence data (28%), manufacturing issues (22%), or labeling errors (18%). If the FDA finds a problem, they issue a Complete Response Letter. Fixing it can add 6 to 12 months to the timeline. And that’s after spending $1.5 million to $3 million on development-for a drug that will sell for pennies on the dollar.

Manufacturing Under the Microscope
The FDA doesn’t just review paperwork. They show up at factories. Every facility that makes generic drugs-whether it’s in the U.S., India, or China-must pass the same inspections as brand-name manufacturers. These are called cGMP (current Good Manufacturing Practices) inspections.Inspectors check everything: how raw materials are stored, whether equipment is cleaned properly, how batches are tested for purity, and whether the final product meets USP <905> standards for uniformity. They take samples. They run tests. They look at the facility’s history. One bad inspection can delay approval for months-or kill the application.
Complex drugs like inhalers, injectable emulsions, or topical creams are especially tricky. In 2022, 45% of rejections for complex generics came from failure to prove equivalence in how the drug was delivered. A generic inhaler might have the same active ingredient, but if the particle size or spray pattern is off, the drug won’t reach the lungs the same way. That’s why the FDA created a Complex Generic Drug Product Initiative-to give clearer guidance and reduce uncertainty for manufacturers.
Real-World Evidence: Do Generics Actually Work?
Some people say, “I switched to the generic, and I didn’t feel the same.” You hear it in pharmacies, online forums, even from doctors. But here’s what the data shows.A 2023 analysis of 15 million patient records by IQVIA found no meaningful difference in outcomes between brand-name and generic versions of common drugs like atorvastatin (for cholesterol) and metformin (for diabetes). In fact, adherence was 3.2% higher with generics-because patients could actually afford to take them.
The FDA’s own adverse event database shows that the rate of reported side effects is nearly identical between brand and generic drugs: 1.6 per million prescriptions for brands, 1.7 for generics. That’s not a difference. That’s noise.
Even the American Medical Association and the Institute of Medicine have confirmed: FDA-approved generics are safe and effective. But there’s one exception: drugs with a narrow therapeutic index-where the difference between a therapeutic dose and a toxic one is tiny. For drugs like warfarin, levothyroxine, or phenytoin, the FDA uses tighter bioequivalence standards: 90% to 111% instead of 80% to 125%. And they maintain a public list of these drugs so prescribers know which ones need extra caution.

Why Some Patients Still Doubt
Despite all this science, 37% of independent pharmacists report patients expressing concerns about generics, especially for neurological or chronic conditions. Why?It’s often about perception. A pill that looks different-different color, shape, or brand name-feels like it might not work the same. Patients who’ve been on the same brand for years may notice a subtle change in how they feel, even if it’s not clinically real. The body adjusts. The brain remembers. And sometimes, that memory overrides the data.
The FDA’s 2020 Patient-Focused Drug Development meeting found that 41% of patients had switched between brand and generic at least once. Only 12% reported feeling the generic didn’t work as well. But when tested objectively, those reports didn’t match blood levels or clinical outcomes. The disconnect isn’t in the drug-it’s in the experience.
The Bigger Picture: Cost, Competition, and Change
Generic drugs save the U.S. healthcare system about $313 billion a year. That’s not a rounding error. It’s enough to cover the entire Medicare Part D program. Without generics, millions of people couldn’t afford their medications.But the system isn’t perfect. The patent landscape is complex. Companies sometimes file dozens of patents on a single drug just to delay generic entry. The FDA’s Orange Book lists over 14,000 patents for brand-name drugs. Challenging them can cost $3 to $5 million in legal fees. That’s why only a few big players-Teva, Viatris, Sandoz-dominate the market. But the FDA is pushing back. Their Generic Drug Competition Action Plan encourages smaller manufacturers to enter the space. In 2022, 55% of approvals went to smaller companies.
And the pressure is growing. Over $260 billion in brand-name drug revenue will lose patent protection between 2024 and 2028. The FDA expects a 25% spike in ANDA submissions. That’s why they’re investing $1.1 billion through GDUFA III to cut review times to 8 months for standard applications-and 6 months for priority ones.
Next up? Biosimilars. The FDA is preparing to approve generic versions of biologic drugs-complex proteins made from living cells-by 2025. That’s a whole new frontier. But the same rules will apply: prove equivalence. Prove safety. Prove it works.
Bottom Line: Trust the System
The FDA doesn’t approve generics because they’re cheap. They approve them because they’ve proven, down to the last decimal point, that they work the same. The process is long, expensive, and intensely scientific. Every batch is tested. Every facility is inspected. Every study is scrutinized.Generics aren’t copies. They’re clones-built to the same exacting standards, tested with the same rigor, and held to the same quality controls as the originals. If your doctor prescribes a generic, you’re not getting second-best. You’re getting the same medicine, at a price that makes treatment possible.
Are generic drugs as effective as brand-name drugs?
Yes. The FDA requires generic drugs to prove bioequivalence-meaning they deliver the same amount of active ingredient into the bloodstream at the same rate as the brand-name version. This is tested in clinical studies with healthy volunteers. Over 90% of prescriptions filled in the U.S. are generics, and studies show no meaningful difference in clinical outcomes for the vast majority of drugs.
Why do generic pills look different from brand-name pills?
By law, generic drugs can’t look exactly like the brand-name version. That’s to avoid trademark infringement. So the color, shape, size, or inactive ingredients (like dyes or fillers) may differ. But the active ingredient, strength, dosage form, and how it works in your body are identical. The difference is cosmetic, not clinical.
Can generic drugs cause more side effects?
No. The FDA’s Adverse Event Reporting System shows that the rate of side effects for generics is statistically identical to brand-name drugs-about 1.6 to 1.7 reports per million prescriptions. If you notice a change after switching, it could be due to differences in inactive ingredients (like a new filler) or psychological factors. Always talk to your pharmacist or doctor if you’re concerned.
Are all generic drugs approved the same way?
Most follow the same ANDA process, but complex drugs like inhalers, injectables, or topical creams require additional testing. The FDA has special guidelines for these, including tighter bioequivalence standards (90-111% instead of 80-125%) for drugs with a narrow therapeutic index, such as warfarin or levothyroxine. These are listed publicly in the FDA’s Narrow Therapeutic Index Drug Product List.
Why do some doctors hesitate to prescribe generics?
Some doctors, especially those treating chronic conditions like epilepsy or thyroid disease, may prefer brands out of habit or because they’ve seen rare patient reports of perceived differences. But the FDA and major medical groups like the American Medical Association confirm generics are safe and effective. For drugs with narrow therapeutic windows, the FDA has stricter standards. If a doctor refuses a generic, ask why-most concerns are based on perception, not evidence.
How long does it take for a generic drug to be approved?
The FDA targets a 10-month review timeline for standard ANDA applications under GDUFA III. But many applications are incomplete or flawed at first-about 35% get a Refuse-to-File letter. Once submitted correctly, the average approval time is 10 to 12 months. Complex drugs or those with patent challenges can take longer, sometimes up to 3-5 years from development to market.
Are generic drugs made in the same factories as brand-name drugs?
Sometimes. Many generic manufacturers use the same facilities as brand-name companies, or even the same production lines. The FDA inspects all facilities equally, regardless of whether they make brand or generic drugs. In fact, over 40% of U.S. generic drug manufacturing occurs in FDA-inspected facilities that also produce brand-name drugs. Location doesn’t determine quality-inspection results do.

Tom Shepherd
November 27, 2025 AT 09:27So if the generic has to hit 80-125% of the brand’s blood levels, that’s a 45% window. That feels wide. I get it’s statistically sound, but what about people who are super sensitive? Like, if I’m on a drug where 5% more or less makes me feel weird, how does that get handled?
Rhiana Grob
November 27, 2025 AT 19:46This is one of the most transparent and well-documented processes in all of pharmaceutical regulation. The FDA doesn’t cut corners just because it’s a generic - they demand the same rigor, just with smarter science. It’s a shame more people don’t understand how much work goes into making these affordable.
Frances Melendez
November 27, 2025 AT 22:44Let’s be real - generics are a scam. Big Pharma and the FDA are in cahoots to keep you hooked on cheap pills while the real medicine gets locked away. My uncle took a generic for his heart and ended up in the ER. Coincidence? I think not. People need to wake up.
shawn monroe
November 29, 2025 AT 22:15Bioequivalence isn’t just a box-ticking exercise - it’s a full-spectrum pharmacokinetic analysis with Cmax, AUC0-t, AUC0-inf, and 90% CI confidence intervals locked down to the decimal. ANDA submissions are monstrous - we’re talking terabytes of raw LC-MS/MS data, PK modeling in Phoenix WinNonlin, and cGMP audit trails that make your head spin. And yes, 35% get Refused-to-File because someone forgot to log a batch number. This isn’t Walmart. This is precision medicine at scale. 🤯
steve stofelano, jr.
November 30, 2025 AT 20:52It is my sincere belief that the FDA’s adherence to the principles of scientific integrity, regulatory transparency, and public health stewardship in the approval of generic pharmaceuticals represents a model of excellence in global regulatory governance. The rigorous application of bioequivalence criteria, coupled with comprehensive manufacturing oversight, ensures that cost-efficiency does not compromise therapeutic efficacy. One is reminded of the adage: 'The measure of a society is how it cares for its most vulnerable.' Generics are not merely economic tools - they are moral imperatives.
Savakrit Singh
December 2, 2025 AT 18:21India produces 40% of global generic volume 🇮🇳. FDA inspects 3,500+ facilities annually - 30% in India. But here’s the kicker: 90% of those Indian facilities pass cGMP. So why do Western patients still distrust generics? 🤔 Because of marketing. Brand names = trust. Generic = 'cheap'. But the pill? Identical. 📊 #PharmaTruth
Cecily Bogsprocket
December 3, 2025 AT 02:25I used to be skeptical too - until my dad switched from the brand-name thyroid med to the generic and his TSH levels didn’t budge. He was scared he’d feel different. He didn’t. He just saved $200 a month. Sometimes the science doesn’t need to be loud to be true. It just needs to be honest. And the FDA? They’re quietly doing the right thing.
Jebari Lewis
December 4, 2025 AT 08:48Frances, your anecdote about your uncle is dangerous misinformation. The FDA’s adverse event database shows no statistically significant difference in side effects between brand and generic drugs. One isolated case does not refute 30 years of population-level data. If you’re going to spread fear, at least cite a peer-reviewed study. Otherwise, you’re not helping - you’re harming.