First-Generation Antihistamines: Why Severe Drowsiness and Anticholinergic Effects Matter
 Dec, 15 2025
Dec, 15 2025
Antihistamine Risk Calculator
How Dangerous Is This Medication For You?
First-generation antihistamines like Benadryl can cause serious side effects including severe drowsiness, impaired driving ability, and long-term cognitive risks. This calculator helps you assess your personal risk level based on your specific circumstances.
Your Risk Assessment
Your Risk Level:
Recommendations:
Most people reach for diphenhydramine (Benadryl) when they have allergies, a runny nose, or trouble sleeping. It’s cheap, easy to find, and works fast. But what most users don’t realize is that this common medication isn’t just making them sleepy-it’s fogging their brain, drying out their mouth, and possibly increasing their risk of memory problems over time. First-generation antihistamines like Benadryl, Chlor-Trimeton, and Phenergan are not the harmless over-the-counter pills they seem. Their side effects aren’t rare exceptions-they’re built into how these drugs work.
Why Do These Medications Make You So Tired?
First-generation antihistamines were designed to block histamine, the chemical your body releases during an allergic reaction. But unlike newer versions, they don’t stop at the site of the allergy. Because they’re small and fat-soluble, they slip right through the blood-brain barrier and start acting on your brain. Once inside, they bind to H1 receptors in areas that control wakefulness, attention, and coordination. This isn’t mild tiredness. It’s deep, drug-induced sedation.
Studies show that after taking a standard 25-50 mg dose of diphenhydramine, brain concentrations reach 15-25 ng/mL within two hours. Compare that to second-generation antihistamines like cetirizine or loratadine, which stay below 1 ng/mL in the brain even at full doses. That’s a 15- to 25-fold difference. The result? Driving simulator tests show first-generation antihistamines impair reaction time as much as having a blood alcohol level of 0.05%. The effects don’t wear off after a few hours-they can linger for up to 18 hours, according to FDA data from 2017 driving studies.
The Hidden Anticholinergic Effects You Can’t Ignore
These drugs don’t just mess with histamine. They also strongly bind to muscarinic receptors-similar to how atropine works. That’s why you get dry mouth, blurry vision, constipation, and trouble urinating. These are anticholinergic effects, and they’re not minor annoyances. They’re signs that the drug is disrupting your nervous system’s ability to regulate basic bodily functions.
For younger people, this might mean needing to sip water constantly or squinting to read a menu. For older adults, it’s far more dangerous. The American Geriatrics Society lists first-generation antihistamines as potentially inappropriate for people over 65. Why? Because long-term use is linked to a 54% higher risk of cognitive decline and dementia. A 2022 study of over 1,200 older adults found that 42% who used diphenhydramine for sleep reported morning confusion lasting 3-4 hours. That’s not normal aging. That’s drug-induced brain fog.
Who Still Uses These-and Why?
Despite the risks, first-generation antihistamines are still everywhere. About 45 million Americans use them every year, mostly as OTC sleep aids or allergy relievers. Their low cost plays a big role: 24 tablets of diphenhydramine cost around $5, while the same number of Zyrtec or Claritin runs $15. For people without insurance or on tight budgets, the price difference is hard to ignore.
They also have niche uses where they still outperform newer drugs. For motion sickness, first-gen antihistamines like dimenhydrinate (Dramamine) are 70-80% effective-far better than second-gen options at 40-50%. They’re also more effective for nausea and vomiting, which is why promethazine is still used in hospitals. And yes, they help people fall asleep faster-by 30-40 minutes on average. But here’s the catch: they don’t improve sleep quality. People wake up groggy, disoriented, and sometimes with urinary retention or dry eyes.

Real People, Real Consequences
Online reviews tell the real story. On Drugs.com, diphenhydramine has a 5.2 out of 10 rating from nearly 4,000 users. Over a third report extreme sleepiness. One Reddit user wrote: “Took Benadryl at 8 PM for hives and woke up at 2 PM the next day feeling like I’d been hit by a truck-not worth it for mild allergies.”
Others report lasting side effects. WebMD forums have dozens of posts from people who’ve used these meds for years and now struggle with urinary problems, memory lapses, or needing artificial saliva because their mouths are always dry. One woman in her late 50s said she started taking diphenhydramine for sleep after menopause. Three years later, she was diagnosed with mild cognitive impairment. Her doctor asked if she’d been using any OTC sleep aids. She hadn’t thought to mention it.
Why the Labels Don’t Tell the Whole Story
Here’s the problem: the warnings on the bottle are buried. The FDA requires drugmakers to include strong warnings about drowsiness, impaired driving, and cognitive effects. But on the actual OTC packaging? The font is tiny. The language is vague. Most users don’t read them-or don’t believe they apply to them.
A 2022 JAMA Internal Medicine study found that 45% of people using first-generation antihistamines underestimated how long the drowsiness would last. Many thought it would wear off by morning. It doesn’t. The impairment can persist for hours after you wake up. That’s why 35% of emergency room visits for drowsy driving involve these medications, according to NHTSA data from 2021.
Who Should Avoid Them Completely?
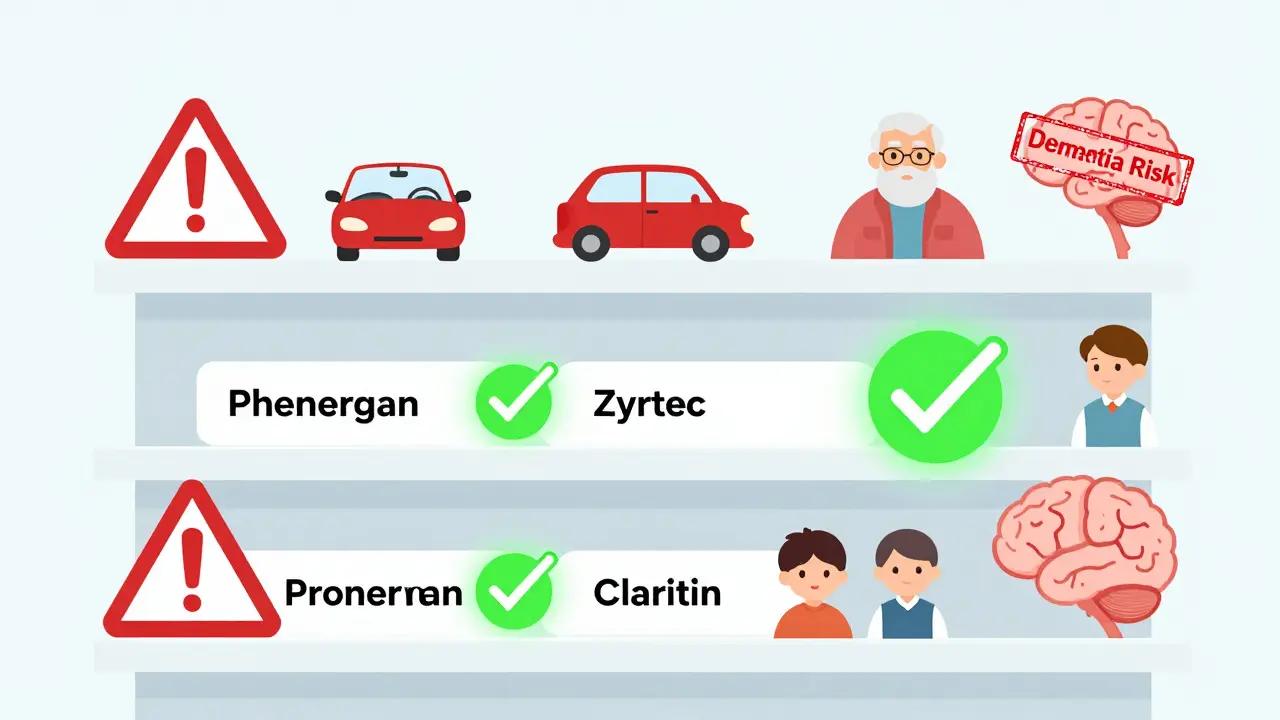
There are clear groups who should never use first-generation antihistamines:
- People over 65-due to dementia risk and increased sensitivity to anticholinergic effects
- Anyone operating machinery or driving-even if they feel “fine”
- People with glaucoma, enlarged prostate, or urinary retention-these drugs can make symptoms worse
- Those taking other sedatives, antidepressants, or pain meds-alcohol and opioids can multiply CNS depression
- Children under 6-the FDA has flagged rising emergency visits linked to misuse in kids
Even if you’re young and healthy, if you need to be alert during the day-whether you’re working, studying, or caring for kids-these drugs are not worth the risk.
What Are the Better Alternatives?
Second-generation antihistamines like cetirizine (Zyrtec), loratadine (Claritin), and fexofenadine (Allegra) work just as well for allergies-but without the brain fog. They’re designed to stay out of the central nervous system. They don’t cause drowsiness in most people, and their effects last 12-24 hours, so you only need to take them once a day.
For sleep, melatonin or cognitive behavioral therapy for insomnia (CBT-I) are safer long-term options. For motion sickness, scopolamine patches are more effective and don’t cause next-day grogginess. For nausea, ondansetron (Zofran) is far better than promethazine.
Yes, these alternatives cost more. But when you factor in lost productivity, increased accident risk, or long-term cognitive damage, the price difference becomes irrelevant.
The Future of Antihistamines
Scientists are already working on the next generation. A 2023 study using cryo-EM imaging identified a new binding site on the H1 receptor. This could lead to drugs that block histamine in the body but can’t cross into the brain. Two candidates, EB-029 and DP-118, are already in Phase II trials and show 80% less brain penetration while keeping full anti-allergy power.
Regulators are catching up too. The UK banned promethazine sales to minors in 2022. The FDA is considering similar restrictions on diphenhydramine after pediatric ER visits rose 27% between 2018 and 2022. The American College of Allergy, Asthma, and Immunology now recommends these drugs only for short-term use in specific cases-like motion sickness or acute insomnia-and only after patients are fully warned.
First-generation antihistamines aren’t going away. But their role is shrinking. They’re no longer the go-to choice for everyday allergies. They’re becoming a last-resort tool-with serious trade-offs.
Are first-generation antihistamines safe for occasional use?
Occasional use-like taking one dose of diphenhydramine for a single night of sleep or a short flight-may be acceptable for healthy adults under 65. But even then, you should avoid driving, operating machinery, or making important decisions for at least 8-12 hours after taking it. The risk isn’t zero. Side effects like dry mouth, blurred vision, and next-day fog can still happen. If you’re using them more than once or twice a month, it’s time to talk to a doctor about safer alternatives.
Can I build up a tolerance to the drowsiness from Benadryl?
Some people report feeling less sleepy after repeated use, but this doesn’t mean the drug is safer. Tolerance to sedation doesn’t mean tolerance to anticholinergic effects. Your brain may adapt to the drowsiness, but your body still experiences dry mouth, constipation, urinary issues, and cognitive strain. Long-term use still increases dementia risk. The sedation may fade, but the damage doesn’t.
Is it safe to mix first-generation antihistamines with alcohol?
No. Alcohol increases how much of the drug enters your brain by 40-60%. This can turn mild drowsiness into dangerous sedation, respiratory depression, or even unconsciousness. Emergency rooms see this combination often-especially in young adults using Benadryl to get high or to enhance alcohol’s effects. The risk of overdose and death rises significantly. Never mix them.
Why do some doctors still prescribe these drugs?
Some doctors prescribe them for motion sickness, severe nausea, or short-term insomnia because they’re effective for those specific uses. But most are aware of the risks. Many are shifting to safer options, especially for older patients. If your doctor prescribes diphenhydramine for chronic allergies or daily sleep, ask if there’s a better alternative. Your health is worth more than the cost difference.
How do I know if I’m experiencing anticholinergic side effects?
Look for these signs: dry mouth that doesn’t go away, trouble urinating or feeling like your bladder isn’t emptying, constipation lasting more than a few days, blurry vision that comes and goes, confusion or memory lapses, or a racing heartbeat. If you’re taking a first-generation antihistamine and notice any of these, stop the medication and talk to your doctor. These aren’t normal side effects-they’re signs your nervous system is being over-suppressed.
If you’ve been using first-generation antihistamines regularly, it’s not too late to switch. Start by replacing one dose at a time with a second-generation option. Track how you feel-your energy, focus, and morning clarity. You might be surprised how much better you feel without the hidden fog.

Hadi Santoso
December 16, 2025 AT 07:17i used to take benadryl every night like it was candy. thought it was just helping me sleep. turns out i was just slowly turning into a zombie. woke up one morning and couldn’t remember where i put my keys… for 20 minutes. dumb as hell.
Mike Smith
December 16, 2025 AT 16:41It is imperative to recognize that the pharmacological profile of first-generation antihistamines presents a significant risk to cognitive integrity, particularly in populations with heightened vulnerability. The data presented here underscores a public health imperative to reevaluate over-the-counter accessibility and labeling protocols.
Ron Williams
December 18, 2025 AT 05:28my grandma took this for years. never thought twice about it. then she started forgetting my name. doctor asked if she was on anything… she said ‘oh, just that little white pill for sleep.’ yeah. that’s the one.
Kitty Price
December 18, 2025 AT 05:51me: ‘just one pill to help me chill’
my brain: *activates dark mode, disables all functions, locks door* 😵💫
Tiffany Machelski
December 19, 2025 AT 21:22why do they even sell this stuff over the counter? i got a headache from just reading this and i’ve never taken it. someone needs to fix this.
James Rayner
December 20, 2025 AT 13:04it’s funny… we’ll warn people about alcohol, cigarettes, even sugar… but this? this quiet, legal, cheap poison? we hand it out like candy at a birthday party. we’re not just ignoring the risk-we’re normalizing it.
Souhardya Paul
December 20, 2025 AT 14:18i switched from benadryl to zyrtec last year. honestly? i didn’t think i’d notice a difference. but my focus at work got better, i didn’t feel like i needed a nap after lunch, and my dry mouth? gone. weird how something so simple can change your whole day.
Josias Ariel Mahlangu
December 21, 2025 AT 11:28people these days. too lazy to just deal with a runny nose. take a pill. take two. now you’re a zombie. this is what happens when you let everyone become their own doctor. you think you’re saving money? you’re just buying a slow death.
anthony epps
December 22, 2025 AT 20:51so… benadryl makes you sleepy. yeah. but it works. i don’t care if my brain feels fuzzy. i just need to sleep.
Andrew Sychev
December 24, 2025 AT 01:44THEY KNOW. THEY KNOW WHAT THEY’RE DOING. THEY’RE SELLING SLEEPY PILLS TO KIDS AND GRANDMAS AND CALLING IT ‘OVER-THE-COUNTER.’ THIS ISN’T MEDICINE. THIS IS A SCAM. AND SOMEONE NEEDS TO GO TO JAIL.
Dan Padgett
December 24, 2025 AT 05:29in my village back home, we used leaves and honey for allergies. now we got pills that make your brain forget your own birthday. progress? nah. just trade one kind of pain for another. and the worst part? nobody even asks why.
Kayleigh Campbell
December 26, 2025 AT 02:49so you’re telling me the same pill that helps me sleep also makes me forget my own phone number? cool. i’ll just keep using it… and blame my bad memory on aging. 😏