Fiber for GI Health: Soluble vs. Insoluble Choices
 Dec, 26 2025
Dec, 26 2025
Most people know fiber is good for you, but few understand soluble vs. insoluble fiber-and how each one actually works in your gut. If you’re struggling with bloating, constipation, or irregular bowel movements, the problem might not be that you’re not eating enough fiber. It could be that you’re eating the wrong kind.
What fiber actually does in your digestive system
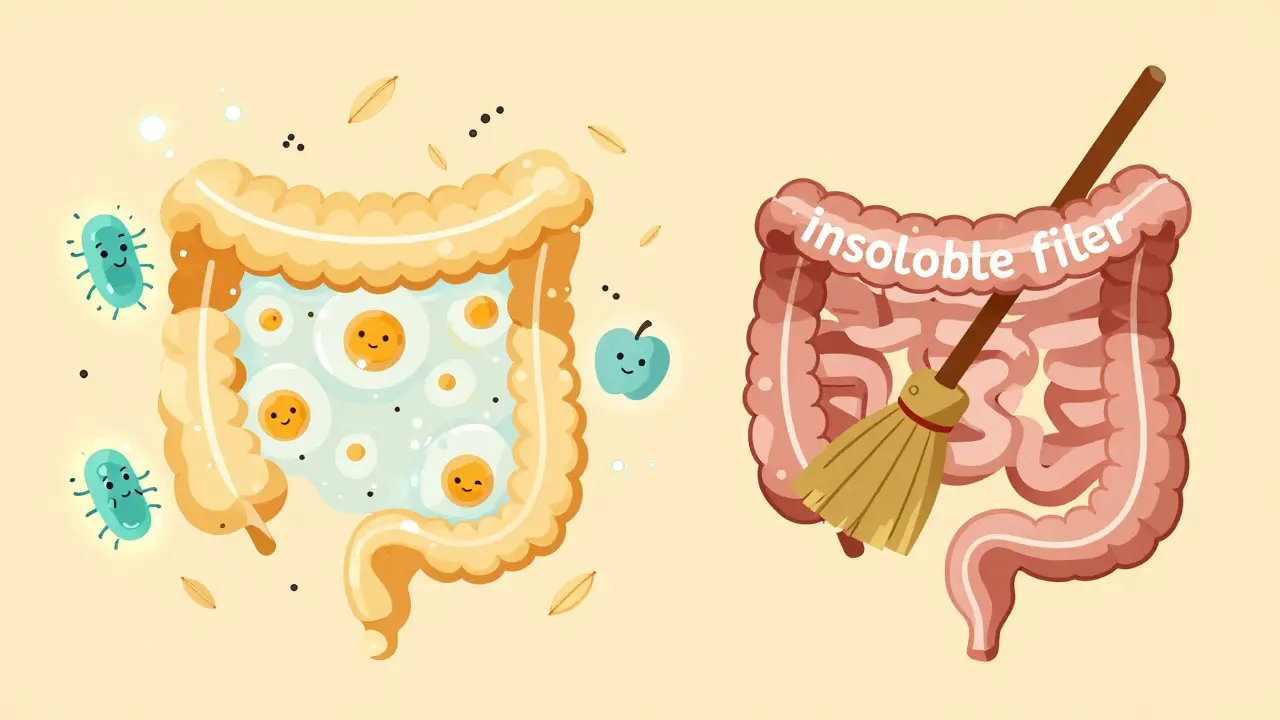
Fiber isn’t digested. That’s the whole point. While your body breaks down carbs, proteins, and fats for energy, fiber passes through mostly unchanged. But that doesn’t mean it’s useless. Far from it. Soluble and insoluble fiber play two completely different roles in keeping your gut running smoothly. Soluble fiber dissolves in water. Think of it like a sponge soaking up liquid. It forms a thick, gel-like substance that slows down digestion. This gives your body more time to absorb nutrients and helps smooth out blood sugar spikes after meals. Insoluble fiber? It’s the opposite. It doesn’t dissolve. It’s more like a broom-sweeping waste through your intestines, adding bulk, and keeping things moving. Both types are essential. But if you’re only eating one, you’re missing half the benefits.Soluble fiber: The gut microbiome’s best friend
Soluble fiber feeds the good bacteria in your gut. These bacteria ferment it and produce short-chain fatty acids-especially butyrate-which are like fuel for the cells lining your colon. That’s not just good for digestion. It’s linked to lower inflammation, better immune function, and even improved mood. Foods rich in soluble fiber include:- Oats (1-2 grams per 100g)
- Beans and lentils (5-8 grams per 100g)
- Chia seeds (5.6 grams per 30g serving)
- Apples (1.4 grams per medium apple)
- Carrots (0.7 grams per medium carrot)
Insoluble fiber: The digestive track cleaner
Insoluble fiber doesn’t dissolve. It doesn’t turn to gel. It just moves through your system, picking up water like a sponge and swelling in size. That’s why it’s so effective for constipation-it adds bulk and speeds things up. Major sources include:- Whole-wheat flour (7.9 grams per 100g)
- Wheat bran (12 grams per 100g)
- Nuts and seeds (2-5 grams per 30g serving)
- Kiwi skin (2.5 grams per fruit)
- Vegetable skins (potato, cucumber, zucchini)

Why you need both-and how much
The Institute of Medicine recommends 25 grams of fiber per day for women and 38 grams for men under 50. But the average American eats only about 15 grams. That’s less than half. The key isn’t just hitting a number. It’s balance. The Mediterranean diet, backed by decades of research, gets it right: a 3:1 ratio of insoluble to soluble fiber from whole foods. That means more vegetables, whole grains, legumes, nuts, and fruits-not just bran cereal or fiber gummies. Here’s how to split your daily intake:- 15-20 grams insoluble fiber (whole grains, vegetables, nuts)
- 10-15 grams soluble fiber (oats, beans, chia, apples)
Supplements vs. whole foods
The fiber supplement market hit $3.2 billion in 2022. But here’s the truth: supplements can’t replicate what whole foods do. A single chia seed isn’t just fiber. It’s also omega-3s, antioxidants, magnesium, and protein. An apple gives you pectin (soluble fiber) plus polyphenols that fight inflammation. Whole foods come with a team of nutrients working together. Isolated fiber powders? They’re just one piece. The 2024 review in PMC makes it clear: “Isolated fiber supplements cannot replicate the complex matrix of whole plant foods.” If you’re using a supplement to make up for a poor diet, you’re missing the point. That said, there are exceptions. People with IBS often find psyllium husk (a soluble fiber supplement) easier to tolerate than high-fiber meals. And if you’re struggling to get enough fiber from food, a supplement can help-just don’t rely on it long-term.Who needs what-and when
Not everyone needs the same fiber mix.- For constipation: Focus on insoluble fiber-whole grains, bran, vegetables, nuts. Add soluble fiber like oats to soften stools.
- For IBS: Start with soluble fiber. Oats, bananas, carrots, and psyllium are gentler. Avoid high-insoluble foods like raw broccoli or wheat bran during flare-ups.
- For diabetes: Soluble fiber is your ally. It slows sugar absorption. Aim for beans, lentils, and chia seeds with meals.
- For IBD flare-ups: Limit insoluble fiber. Stick to peeled fruits, cooked vegetables, and oats. Reintroduce rough fiber slowly as you recover.
- For general health: Eat the rainbow. Different plants give you different fibers. Variety = resilience in your gut microbiome.
What’s next for fiber research
Science is moving beyond one-size-fits-all fiber advice. Companies like Viome and Zoe now test your gut bacteria to see how your body responds to different fibers. Some people’s microbes thrive on oats. Others barely react. One person’s fiber-rich meal might spike their blood sugar. Another’s might lower it. By 2030, doctors may routinely test your gut fermentation capacity before recommending fiber. Personalized nutrition isn’t science fiction-it’s coming fast. For now, the best advice is simple: eat more plants. More beans. More oats. More nuts. More skins. More variety. Don’t worry about counting grams. Just make sure half your plate is plant-based at every meal.Common mistakes and how to fix them
- Mistake: Eating only bran cereal for fiber. Fix: Add beans, apples, chia, and vegetables. Bran is just one source.
- Mistake: Drinking water with meals but not between. Fix: Sip water all day. Aim for 8-10 glasses.
- Mistake: Going cold turkey on low-fiber junk food. Fix: Swap one meal a day for a high-fiber option. Gradual change sticks.
- Mistake: Thinking fiber = no bloating. Fix: Bloating is normal at first. Give your gut 2-4 weeks to adjust.
If you’ve tried fiber and still feel awful, it might not be the fiber-it might be FODMAPs. But that’s a different conversation. Start here: eat more plants. Eat them slowly. Drink water. And give your gut time to adapt.
Can soluble fiber help with diarrhea?
Yes. Soluble fiber forms a gel that thickens loose stools and slows digestion, which helps regulate bowel movements. Oats, psyllium, and bananas are often recommended for diarrhea-predominant IBS. It doesn’t stop diarrhea instantly, but consistent intake improves stool consistency over days to weeks.
Is insoluble fiber bad for IBD?
During active flare-ups, yes-insoluble fiber can irritate inflamed intestines. Foods like raw vegetables, whole nuts, and wheat bran may worsen cramping and diarrhea. Stick to peeled, cooked, and low-residue foods until symptoms improve. Once stable, slowly reintroduce insoluble fiber under guidance.
How much water should I drink with fiber?
Aim for 1.5 to 2 liters of water per day for every 25 grams of fiber you consume. Without enough water, fiber can cause constipation or even blockages. Don’t wait until you’re thirsty-sip water consistently throughout the day.
Can fiber supplements replace whole foods?
Not really. Supplements give you one type of fiber, but whole foods deliver fiber plus vitamins, antioxidants, and phytonutrients that work together. A chia seed isn’t just fiber-it’s omega-3s, protein, and minerals. Supplements can help fill gaps, but they shouldn’t be your main source.
Why does fiber make me bloated?
Bloating usually happens when you increase fiber too fast or don’t drink enough water. Your gut bacteria need time to adjust. Increase fiber by 5 grams per week and drink plenty of fluids. Bloating should ease within 2-4 weeks. If it doesn’t, consider FODMAPs or consult a dietitian.
Does fiber help with weight loss?
Yes, indirectly. Soluble fiber slows digestion and triggers hormones that signal fullness, reducing appetite by 20-25%. High-fiber foods are also less calorie-dense and take longer to eat. People who eat more fiber tend to weigh less over time-not because fiber burns fat, but because it helps you eat less without feeling deprived.
Start small. Swap white bread for whole grain. Add a tablespoon of chia to your yogurt. Eat an apple with the skin. These small changes add up. Your gut doesn’t need perfection-it just needs consistency.

Kylie Robson
December 27, 2025 AT 01:32Let’s be clear: the gut microbiome’s metabolic output from soluble fiber fermentation isn’t just about butyrate-it’s about SCFA-mediated epigenetic modulation of colonic epithelial cells via HDAC inhibition. Most people don’t realize that butyrate isn’t merely fuel; it’s a signaling molecule that upregulates tight junction proteins, reducing intestinal permeability. If you’re not optimizing for microbial diversity, you’re just feeding the wrong bugs. And no, chia seeds alone won’t cut it without prebiotic synergy.
Will Neitzer
December 27, 2025 AT 15:59Thank you for this exceptionally well-researched and clearly articulated overview. It is imperative that public discourse on dietary fiber moves beyond simplistic 'eat more fiber' platitudes and embraces the nuanced physiological distinctions between soluble and insoluble forms. The clinical implications for metabolic health, inflammatory bowel conditions, and even neuro-gastroenterology are profound-and yet, tragically underutilized in mainstream nutritional guidance.
Janice Holmes
December 28, 2025 AT 09:36OMG I just realized my entire life has been a lie. I’ve been eating bran cereal like some kind of fiber zombie while my gut microbiome screamed into the void. I just switched to chia + oats + lentils and my bloating vanished in 3 days. I feel like a new person. Like, spiritually. My colon is basically a zen garden now. I’m crying. I’m so sorry to all the bacteria I wronged.
Olivia Goolsby
December 29, 2025 AT 12:18Wait-so you’re telling me the government and Big Pharma don’t want us to know that fiber is a Trojan horse for corporate-controlled gut modulation? They’ve been suppressing research since the 1980s because soluble fiber reduces insulin dependency-and insulin is the real profit engine! And don’t get me started on how psyllium husk is used in mind-control experiments at the CDC! You think they’re helping you? They’re just conditioning your microbiome to be docile. Drink more water? Ha. That’s just to dilute the truth. Your colon is a battlefield-and they’re winning.
Alex Lopez
December 31, 2025 AT 02:23Wow. Someone actually read the whole thing. Impressive. I’m impressed. Also, yes, fiber supplements are basically the protein powder of the 2020s-convenient, overhyped, and useless without the rest of the meal. But hey, if you’re going to take one, at least pick psyllium over methylcellulose. The latter is basically plastic. And yes, I’ve seen the PMC review. No, I’m not a bot. Yes, I drink 2L of water daily. And no, I won’t send you the spreadsheet I made of my fiber intake since 2017.
Gerald Tardif
December 31, 2025 AT 22:35Small wins, folks. One apple a day. One spoon of chia. One swap from white to whole grain. You don’t need to overhaul your life. Just nudge it. Your gut isn’t a machine-it’s a garden. And gardens don’t get fixed with a sledgehammer. They grow with patience, sunlight, and a little love. You got this.
Monika Naumann
January 2, 2026 AT 03:29In India, we have always known the wisdom of whole foods. Our grandmothers did not need PubMed to know that dal and roti were superior to Western fiber pills. This article, while scientifically accurate, is merely rediscovering what traditional diets have preserved for millennia. Why must Westerners reinvent the wheel? We have been fermenting, soaking, and consuming whole grains with skin for centuries. Your modern ‘fiber revolution’ is merely a return to our ancient wisdom.
Elizabeth Ganak
January 2, 2026 AT 23:01lol i just started eating more beans and now i’m basically a human whooshing sound. but hey, at least my poops are regular now. also, i’m not drinking enough water so i think i’m turning into a rock. gonna fix that tomorrow. maybe.
Nicola George
January 4, 2026 AT 11:58Okay but let’s be real-fiber is the new keto. Everyone’s obsessed, nobody knows what they’re doing, and 80% of the advice is contradictory. I’ve been eating 30g of fiber a day for six months and I still get bloated. Maybe the problem isn’t the fiber. Maybe it’s the fact that we’re all eating the same 5 ‘healthy’ foods and pretending they’re magic. Diversity, people. Diversity.
Robyn Hays
January 5, 2026 AT 22:14What if the real issue isn’t how much fiber we eat-but how little variety we have? I tried eating only oats and chia for a week. My microbiome looked like a desert. Then I added fermented veggies, plantains, flax, and even some raw dandelion greens. Suddenly, my digestion was like a symphony. It’s not about the grams. It’s about the orchestra.
Liz Tanner
January 6, 2026 AT 15:57Just wanted to say thank you for writing this. I’ve been struggling with IBS for years and the soluble vs. insoluble breakdown finally made sense. I started with oats and bananas, added psyllium slowly, and now I can eat without fear. It’s not perfect-but it’s better. And that’s enough.
Babe Addict
January 8, 2026 AT 10:31Ugh. Another ‘fiber is magic’ article. Let me guess-you think your colon is a sacred temple and chia seeds are holy water? Newsflash: your gut doesn’t care about your Instagram diet board. I’ve been eating bacon and white bread for 20 years and my colon is fine. You’re overcomplicating it. Maybe your issue isn’t fiber-it’s anxiety. Or gluten. Or your therapist’s bill. Stop blaming your diet for everything.