Crohn’s Disease: Managing Chronic Inflammation with Biologic Therapy
 Jan, 28 2026
Jan, 28 2026
For someone living with Crohn’s disease, the daily reality isn’t just stomach pain or frequent bathroom trips. It’s the unpredictability - one day you feel okay, the next you’re in the hospital. The inflammation doesn’t just sit in your gut; it rewires your life. But over the last 25 years, a new class of drugs has changed everything: biologic therapy.
What Makes Crohn’s Disease Different?
Crohn’s disease isn’t just ‘bad IBS.’ It’s a chronic autoimmune condition where your immune system attacks your own digestive tract, causing deep, painful inflammation that can show up anywhere from your mouth to your anus. About 70-80% of cases involve the end of the small intestine and the beginning of the colon. This isn’t surface-level irritation - it’s transmural inflammation, meaning it cuts through all layers of the intestinal wall. That’s what leads to complications like strictures (narrowing), fistulas (abnormal tunnels), and abscesses.It’s not caused by diet or stress alone. Genetics play a big role. If you have a close relative with Crohn’s, your risk jumps significantly. Over 200 genes have been linked to the disease, with mutations in the NOD2/CARD15 gene found in up to 40% of families with a history. Environmental triggers - like smoking, antibiotics in childhood, or a Western diet high in processed foods - can turn those genetic risks into active disease.
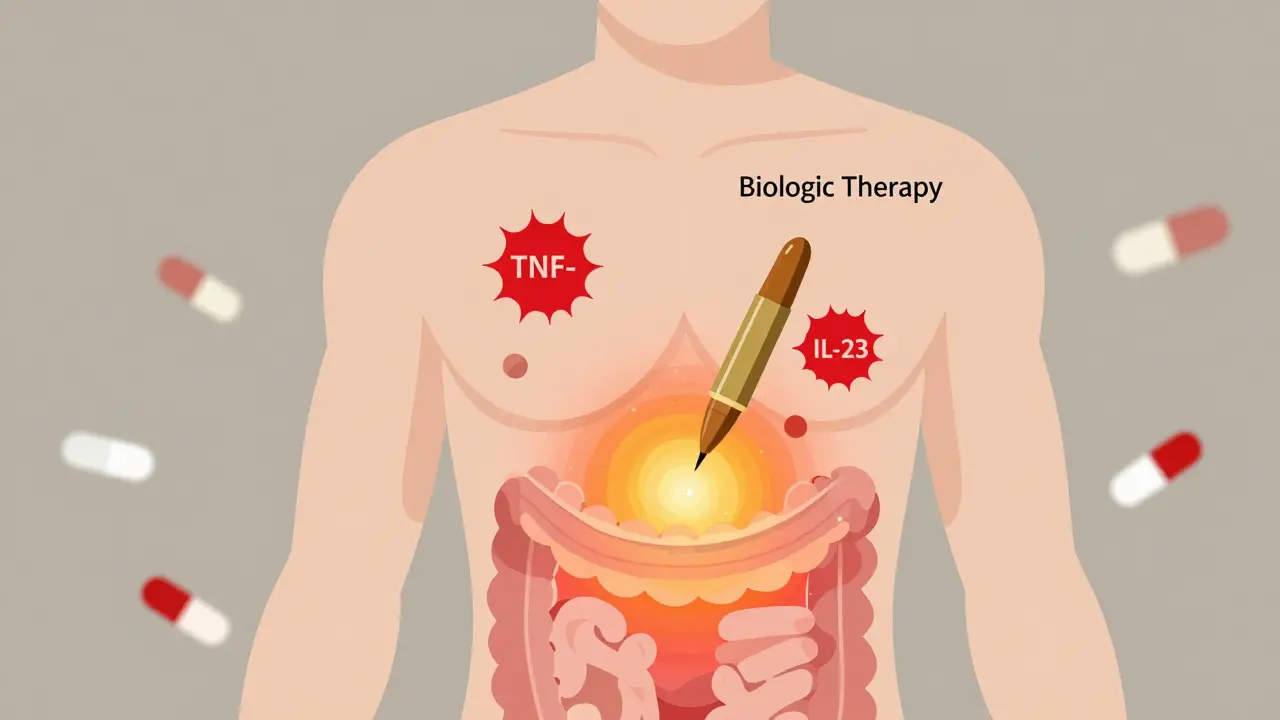
The real problem? Your immune system gets stuck in overdrive. Immune cells flood your gut, releasing inflammatory chemicals like TNF-alpha, IL-12, and IL-23. These aren’t just bystanders - they’re the main drivers of tissue damage. And once this cycle starts, it doesn’t just stop on its own.
Why Conventional Treatments Often Fall Short
For decades, doctors relied on steroids like prednisone to calm flares. They work - fast. But they’re like a fire extinguisher on a gas leak. They mask the problem without fixing it. Long-term steroid use brings weight gain, bone loss, diabetes, and mood swings. Not worth it.Immunomodulators like azathioprine or methotrexate were next. They take months to work and still only help about half the people who try them. Plus, they suppress your whole immune system, increasing infection risk without targeting the root cause.
That’s where biologics changed the game. Instead of blanket immune suppression, they’re precision tools. They zero in on specific molecules that fuel inflammation - like a sniper instead of a bomb.
The Biologic Arsenal: How Each One Works
There are now five main types of biologics approved for Crohn’s disease. Each targets a different part of the inflammatory process.- Anti-TNF agents (infliximab, adalimumab, certolizumab, golimumab): These block tumor necrosis factor-alpha, the most studied and widely used target. They’re the first-line biologic for most moderate-to-severe cases. Around 30-40% of patients achieve remission with them, compared to just 15-20% on placebo.
- Vedolizumab: This one doesn’t touch the whole immune system. It blocks α4β7 integrin - a protein that only lets immune cells enter the gut. That’s why it’s called ‘gut-selective.’ Only 4% of patients develop antibodies against it, compared to 15-20% with anti-TNF drugs. But it takes longer to work - 10 to 14 weeks vs. 2 to 4.
- Ustekinumab: Targets IL-12 and IL-23, two key cytokines driving inflammation. In clinical trials, 34-44% of patients went into remission at 8 weeks. What’s impressive? About half of those patients stayed in remission after a year.
Biosimilars - cheaper copies of original biologics like infliximab-dyyb - are now widely available. They work the same way, with similar safety profiles. Many insurance plans now push for biosimilars first to cut costs.
Who Gets Biologics - And When?
The old way was ‘step-up’: start with mild meds, escalate only if they fail. Now, experts push for ‘top-down’ - starting with biologics early if you’re at high risk.Who’s high risk? If you’re diagnosed with deep ulcers, strictures, fistulas, or perianal disease, you’re in that group. Studies show patients who start biologics early have a 50% lower chance of needing surgery within five years.
Guidelines from the European Crohn’s and Colitis Organisation (ECCO) and the American College of Gastroenterology now support this approach. If your disease is moderate to severe at diagnosis, skipping straight to a biologic isn’t reckless - it’s smart.
But not everyone needs them. Mild cases, especially if they respond well to diet changes or mesalamine, might not need biologics right away. The goal isn’t to treat everyone - it’s to treat the right people at the right time.
Therapeutic Drug Monitoring: The Secret to Success
One of the biggest mistakes patients make? Assuming that if the drug worked once, it’ll always work. But many lose response over time. Why? Your body starts making antibodies against the drug.That’s where therapeutic drug monitoring comes in. Doctors now check your blood levels of the drug (trough levels) and look for antibodies. For infliximab, the sweet spot is 3-7 μg/mL. For adalimumab, it’s 5-12 μg/mL. If you’re below that, your dose might need to be increased or given more often. If antibodies are high, switching to another biologic - like from an anti-TNF to vedolizumab - often helps.
Studies show patients who get their levels checked and adjusted have 3.5 times higher remission rates than those who don’t. It’s not optional anymore - it’s standard care.
Real-Life Outcomes: What Patients Actually Experience
On Reddit’s r/Crohns_Disease community, one user wrote: “After 15 bowel movements a day and failing three other drugs, infliximab cut it to two in three infusions.” That’s not an outlier. In a 2023 survey of over 1,200 patients, 78% said biologics improved their quality of life. Hospitalizations dropped by 72%. Most stopped needing steroids - 85% of users achieved steroid-free remission.But it’s not all smooth sailing. About 35% report injection or infusion reactions - redness, itching, chills. Around 28% worry about long-term infection risks. One patient developed a lupus-like reaction after 18 months on Humira and needed six months of steroids to recover.
Cost is another huge barrier. Annual treatment can run $40,000 to $70,000. In the same survey, 40% of patients delayed doses because their copay was over $150 per injection or infusion. Patient assistance programs exist - some cover 30-50% of out-of-pocket costs - but navigating them takes time and support.

What Happens Before You Start
You can’t just walk in and get a biologic. There’s a checklist.- Tuberculosis test (QuantiFERON Gold)
- Hepatitis B and C screening
- Heart function check (some biologics can worsen heart failure)
- Vaccinations - especially live vaccines like MMR or varicella - must be up to date before starting
For subcutaneous biologics like adalimumab or ustekinumab, you’ll need training on self-injection. Most patients master it after two or three supervised sessions. For infliximab or vedolizumab, you’ll go to a clinic every 8 weeks for an infusion that takes about two hours.
Many clinics now use IBD nurse specialists to guide patients through this process. They help with scheduling, managing side effects, and connecting you to financial aid programs. Mobile apps like MyIBDCoach are also popular - 45% of users track symptoms, meds, and bowel habits to spot flares early.
What’s Next? Emerging Treatments
The pipeline is full. Ozanimod, a pill that traps immune cells in lymph nodes, showed 37% remission in a 2021 trial. Mirikizumab, which blocks only IL-23 (not IL-12), hit 40% endoscopic improvement in phase 3 studies. Both could be approved by 2027.Biosimilars are already making biologics more affordable. IMS Health predicts prices could drop 15-30% over the next five years. That’s huge for patients who’ve been forced to skip doses because of cost.
But the biggest shift isn’t just new drugs - it’s better timing. We’re moving from treating flares to preventing them. The goal isn’t just symptom control anymore. It’s mucosal healing - actually repairing the gut lining. Biologics are the only class of drugs that consistently achieve this, with healing rates of 40-60% compared to 20-30% with older drugs.
Final Thoughts: It’s Not a Cure - But It’s a Lifeline
Crohn’s disease still has no cure. But biologic therapy has turned it from a life-limiting condition into a manageable one. For many, it means going back to work, traveling, having kids, living without constant pain.It’s not easy. Injections, infusions, blood tests, insurance battles - it’s a lot. But the data is clear: if you’re a good candidate, starting a biologic early gives you the best shot at long-term remission, fewer surgeries, and a real life outside the bathroom.
Don’t wait until you’re in the ER to ask about options. Talk to your gastroenterologist about your goals - not just symptom control, but healing, function, and freedom. The tools are here. You just have to use them.

Keith Oliver
January 28, 2026 AT 16:33Bro, I’ve been on Humira for 3 years and honestly? It’s the only thing keeping me from living in a bathroom. I used to miss work every other week. Now I hike on weekends. No cap. The injections suck but the freedom? Priceless.
Kacey Yates
January 29, 2026 AT 01:12biologics saved my life but the cost is a joke my insurance made me switch to a biosimilar then my trough levels dropped i had to beg for a prior auth for 3 months and now i’m back on the original just to not be in pain again
ryan Sifontes
January 30, 2026 AT 10:13they say it works but what about the cancer risk i mean i saw a guy on youtube who got lymphoma after 5 years on infliximab and now he’s gone what if that’s me next
Laura Arnal
January 31, 2026 AT 16:14you’re not alone 💪 i was scared to start biologics too but my nurse walked me through every step and now i’m back to cooking for my kids 🥹 trust the process it’s hard but worth it
Pawan Kumar
February 2, 2026 AT 04:16While the pharmacological intervention of biologics is undeniably efficacious, one must interrogate the underlying epistemological framework of modern gastroenterology. The reductionist paradigm of cytokine blockade fails to account for the holistic dysbiosis inherent in Crohn’s pathology. One must ask: is this not merely symptom suppression masquerading as therapeutic triumph? The gut microbiome, a complex ecosystem, is reduced to a chemical target. This is not medicine. It is pharmacological colonialism.
Jasneet Minhas
February 3, 2026 AT 09:14biologics? more like biologic propaganda. 🤡 next they’ll tell us to take a pill for breathing too hard. i’ve been on 3 of these and my gut still screams at me. the real cure? quit sugar. and stop drinking that ‘gut health’ kombucha nonsense.
DHARMAN CHELLANI
February 4, 2026 AT 12:27biologics are just big pharma’s way to keep you hooked. they dont cure they rent. same as antidepressants. you think you’re fixed? nah you’re just paying monthly.
Eli In
February 5, 2026 AT 00:17as someone from a country where this stuff isn’t even covered… i’m so grateful people here have access. i know it’s expensive and scary but please don’t give up. i’ve seen friends go from wheelchairs to walking again. 🌍❤️
Sheryl Dhlamini
February 5, 2026 AT 02:40i just want to say thank you to whoever wrote this. i’ve been living with this for 12 years and no one ever explained it like this. i finally feel seen. i’m going to print this out and give it to my doc tomorrow.
kabir das
February 5, 2026 AT 03:05...and yet... you still don't know... what happens... when the antibodies... develop... and the drug... stops working... and you're left... with nothing... but a hole... in your gut... and a debt... you'll never pay off... and a doctor... who just shrugs... and says... 'try the next one'...?