Cerebral Aneurysm: Understanding Rupture Risk and Modern Treatment Choices
 Nov, 19 2025
Nov, 19 2025
What Is a Cerebral Aneurysm?
A cerebral aneurysm is a weak, bulging spot in a brain artery. Think of it like a balloon forming on a garden hose - the wall of the vessel stretches thin and fills with blood. Most people don’t know they have one until it ruptures or is found by chance during imaging for another reason. Around 3.2% of adults worldwide have at least one unruptured brain aneurysm, according to large-scale studies. The real danger isn’t the bulge itself - it’s the chance it bursts. When that happens, it causes a subarachnoid hemorrhage, a type of stroke that bleeds into the space around the brain. About 30 to 40% of people die within the first day after rupture. Survivors often face long-term disability.
Who’s at Risk for Rupture?
Rupture risk isn’t random. It’s shaped by a mix of things you can’t change and things you can.
- Age: After 65, your rupture risk jumps 2.7 times compared to younger adults.
- Gender: Women are 1.6 times more likely than men to develop aneurysms, and they’re more likely to rupture.
- Family history: If two or more close relatives had one, your risk is four times higher.
Modifiable risks are where you have control:
- High blood pressure: Systolic pressure over 140 mmHg makes rupture 2.3 times more likely.
- Smoking: Current smokers face a 3.1 times higher risk. If you smoke 10 or more cigarettes a day, that risk climbs another 47%.
- Alcohol: More than 14 drinks a week increases rupture risk by 32%.
These aren’t just statistics - they’re warning signs. Quitting smoking cuts rupture risk by 54% within two years. Controlling blood pressure isn’t optional - it’s the single most effective way to prevent rupture if you have an unruptured aneurysm.
What Makes an Aneurysm More Likely to Burst?
Not all aneurysms are created equal. Size, shape, and location matter more than you might think.
- Size: Aneurysms 7 mm or larger have a 3.1 times higher chance of rupturing than smaller ones.
- Shape: Irregular shapes - especially those with daughter sacs (small bulges off the main one) - increase rupture risk by 68%. Spherical aneurysms are far more stable.
- Location: Some spots are danger zones. The anterior communicating artery (AComm) is notorious - even small aneurysms here rupture more often. Middle cerebral artery aneurysms carry a 3.6 times higher risk. Distal anterior cerebral artery aneurysms can burst even if they’re under 5 mm.
These aren’t guesses. They’re backed by data from thousands of patients tracked over years. A 2021 JAMA Neurology study showed that irregular shape alone raised rupture risk by 2.9 times. Another study found that 83% of ruptured aneurysms had abnormal blood flow patterns - low or swirling shear stress - compared to only 42% of unruptured ones.
The PHASES Score: Your Personalized Rupture Risk Calculator
Doctors don’t just guess whether an aneurysm will burst. They use tools - and the most trusted one is the PHASES score. It combines six factors:
- P - Population (where you live)
- H - Hypertension
- A - Age
- S - Size
- E - Earlier subarachnoid hemorrhage
- S - Site (location)
Each factor adds points. A total score of 0-3 means your 5-year rupture risk is just 3%. A score of 9-10? That’s a 45% chance. Every single point increase raises your risk by 32%. If your score is 6 or higher, most neurosurgeons recommend treatment. Below 6? Monitoring may be safer.
There’s also the ELAPSS score and the triple-S model (size, site, shape), which help predict risk over shorter periods - like 6 months or a year. These aren’t just academic tools. They’re used daily in hospitals to decide who needs surgery and who can wait.
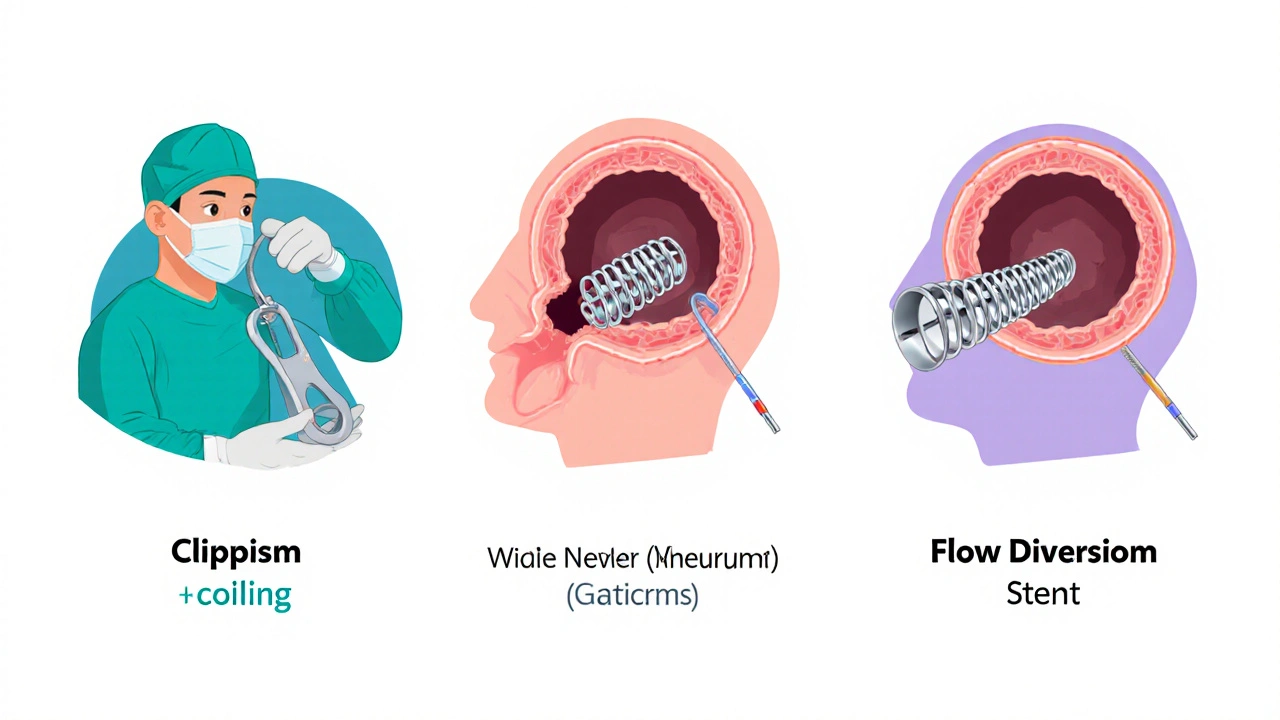
Treatment Options: Clipping, Coiling, and Flow Diversion
If treatment is needed, you have three main choices.
1. Surgical Clipping
This is the original method, first done in 1937. A neurosurgeon opens the skull (craniotomy), finds the aneurysm, and places a tiny titanium clip across its neck. It’s like pinching a balloon shut at the base. Success rates are high - 95% of aneurysms are fully sealed. Long-term, 88-92% stay closed for life. But it’s invasive. Recovery takes weeks. People over 70 have a 35% higher risk of complications.
2. Endovascular Coiling
First done in 1991, coiling is less invasive. A catheter is threaded from the groin up to the brain. Platinum coils are packed into the aneurysm, triggering a clot that seals it off. Success at 6 months: 78-85%. The big advantage? Shorter hospital stays and faster recovery. But there’s a catch: 15.7% of coiled aneurysms need retreatment within 12 years, compared to just 6.2% for clipped ones. Still, the 1-year death rate is 22.6% lower than with clipping.
3. Flow Diversion
This is the newest option. A porous stent (like the Pipeline Embolization Device) is placed in the artery, redirecting blood away from the aneurysm. Over time, the aneurysm shrinks and seals itself. It’s especially good for large, wide-necked, or complex aneurysms. At 6 months, 76.4% are fully occluded. At 1 year, newer models like the PED-PLATINIUM show 85.5% success. But it takes months for the aneurysm to fully close - so you need to stay on blood thinners. Complication rates are slightly higher than coiling, but mortality is the lowest of all three.
What About the WEB Device?
For aneurysms at the base of blood vessel branches (bifurcations), there’s a newer tool called the WEB (Woven EndoBridge). Approved in 2019, it’s a mesh sphere that sits inside the aneurysm and blocks blood flow. In the WEBCAST trial, 71.4% were completely sealed at 1 year. It’s not for every aneurysm - only specific shapes and locations - but it’s a big step forward for tricky cases.
Medical Management: What You Can Do Right Now
Not every aneurysm needs surgery. Small ones in low-risk areas - especially under 5 mm - can be watched. The UCAS Japan study found that posterior circulation aneurysms under 5 mm had only a 0.7% chance of rupturing in 5 years. Anterior ones? Just 0.2%.
That means medical management isn’t passive. It’s active prevention:
- Keep blood pressure under 130/80 - this is non-negotiable.
- Quit smoking - the benefits start within weeks.
- Limit alcohol - no more than 7 drinks a week is safer.
- Annual MRA scans - to check for growth or shape changes.
These steps don’t just lower rupture risk - they improve your overall brain health. Even if you never need surgery, this is the best way to protect yourself.
Complications and Long-Term Outcomes
Every treatment has risks:
- Clipping: 4.7% permanent disability, 1.5% death
- Coiling: 3.9% permanent disability, 1.1% death
- Flow diversion: 5.2% permanent disability, 0.8% death
Long-term, successful treatment cuts the 10-year re-rupture risk from 68% down to just 2.3%. Quality of life is better after coiling - patients report higher scores on the EQ-5D scale (0.82 vs. 0.76 for surgery at 1 year). Recovery isn’t just about survival. It’s about returning to your life - working, walking, laughing - without constant fear.
What’s Next in Research?
Scientists aren’t stopping. The HUNT study found 17 genetic markers linked to aneurysm formation and rupture. Blood tests for these markers could one day predict who’s at highest risk before an aneurysm even forms.
Machine learning is also stepping in. New models analyze 42 different features - shape, flow patterns, wall thickness - to predict rupture better than PHASES alone. In 2024, researchers showed these AI tools could improve accuracy by up to 18%.
The goal isn’t just to treat aneurysms. It’s to stop them before they happen.
When to Seek Help
If you have a known unruptured aneurysm, stick to your monitoring plan. Don’t skip scans. If you’ve never been diagnosed but suddenly get the worst headache of your life - like something "exploding" in your head - get to the ER immediately. That’s the classic sign of rupture. So is nausea, stiff neck, blurred vision, or loss of consciousness.
Don’t wait. Don’t assume it’s a migraine. Time is brain - and with aneurysms, every minute counts.

Matthew Peters
November 20, 2025 AT 07:16Liam Strachan
November 20, 2025 AT 12:11Gerald Cheruiyot
November 22, 2025 AT 06:52Michael Fessler
November 23, 2025 AT 07:23daniel lopez
November 24, 2025 AT 10:00Nosipho Mbambo
November 24, 2025 AT 14:25Katie Magnus
November 25, 2025 AT 14:36King Over
November 26, 2025 AT 05:07Johannah Lavin
November 28, 2025 AT 03:07Matthew Karrs
November 29, 2025 AT 20:19Ravi boy
November 30, 2025 AT 02:20