Autoimmune Disorder Medications: Understanding Immunosuppression Complications
 Jan, 22 2026
Jan, 22 2026
Immunosuppressant Vaccine Timing Calculator
How to Use This Tool
Enter your immunosuppressant medication and vaccination status to calculate safe vaccine timing windows. Based on CDC guidelines and medical research.
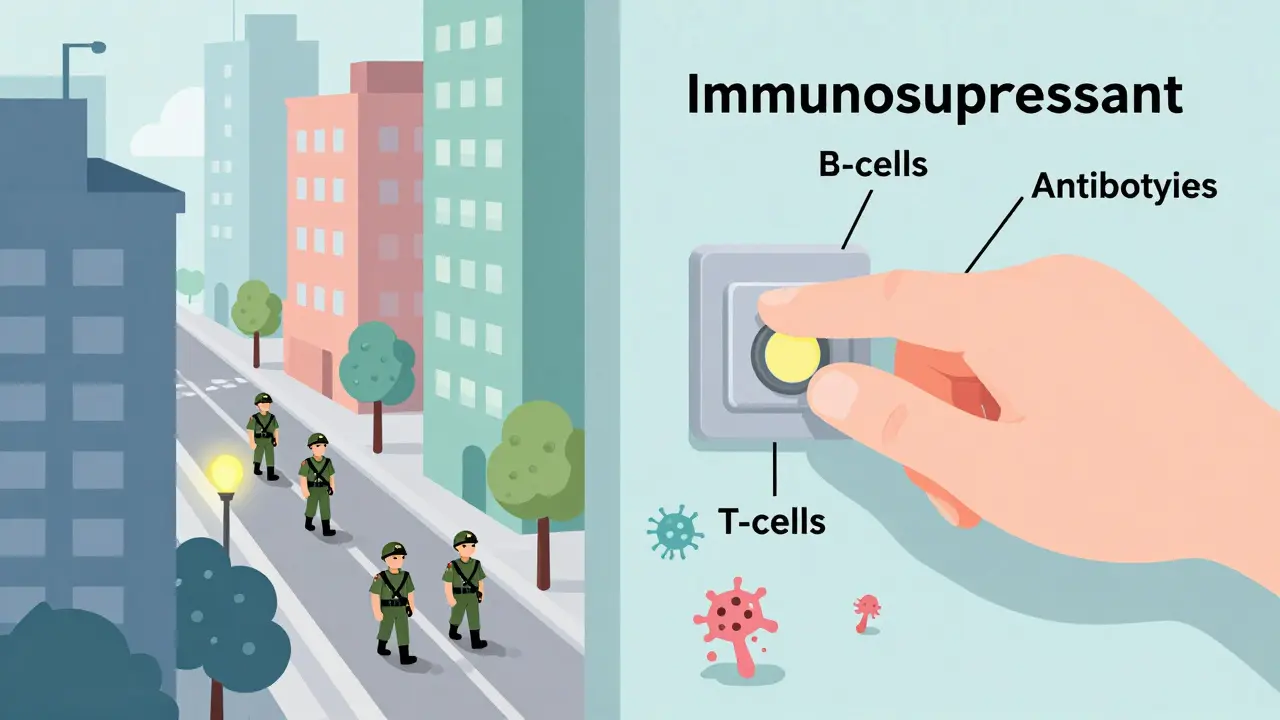
When you're managing an autoimmune disorder like rheumatoid arthritis, lupus, or Crohn’s disease, the goal is simple: stop your immune system from attacking your own body. But the drugs that do this-immunosuppressants-don’t just turn off the bad parts of your immune system. They turn down the whole thing. And that’s where things get dangerous.
What Immunosuppressants Actually Do
These medications don’t cure autoimmune diseases. They suppress the immune response enough to slow damage to joints, skin, intestines, or organs. But because your immune system protects you from infections and cancer, weakening it comes with serious trade-offs. The CDC estimates over 5 million Americans are on these drugs right now, and that number is growing every year. The problem isn’t the drugs themselves-it’s how little most people understand what they’re really signing up for.
There are six main types of immunosuppressants, and each has its own risk profile. Corticosteroids like prednisone are the oldest and most widely used. They work fast, but if you’re on more than 20 mg a day for over two weeks, your risk of serious infections jumps dramatically. Even after you stop taking them, your immune system can stay down for weeks. That’s why people on long-term steroids get pneumonia or fungal infections they shouldn’t have.
The Hidden Dangers of Biologics
Biologics like Humira, Remicade, and Rituxan were supposed to be smarter. They target specific parts of the immune system instead of blasting everything. But they’re not safer-they’re just different. Rituximab, for example, wipes out B-cells, which are crucial for fighting off viruses and making antibodies. After one course, it can take up to six months for your body to rebuild them. During that time, you’re wide open to infections you’d normally shrug off.
One patient on Reddit shared how he got shingles four months after his second Rituxan infusion. His doctor never warned him about the six-month window of vulnerability. That’s not rare. Studies show 1.8% of people on Rituxan get hepatitis B reactivated-even if they were cleared before treatment. And in rare cases, a brain infection called PML can develop. It’s deadly. The risk is low-about 0.07 per 1,000 patients-but when it happens, there’s no second chance.
JAK Inhibitors: The New Risk
JAK inhibitors like Xeljanz and Olumiant are oral drugs that replaced some biologics because they’re easier to take. But they come with their own set of red flags. The FDA issued a black box warning in 2021 after studies showed these drugs increase the risk of blood clots, heart attacks, and certain cancers. People over 65 who smoke are especially at risk for lymphoma and lung cancer. One study found a 1.44-fold increase in lymphoma risk compared to TNF blockers.
And then there’s shingles. JAK inhibitors cause 3 to 5 cases per 100 patients each year-much higher than older drugs. Even if you’ve had chickenpox before or got the vaccine, the virus can come back with a vengeance. A nurse with rheumatoid arthritis on HealthUnlocked said she checks her varicella zoster antibody levels every six months now, just to be safe.

How Other Drugs Stack Up
Not all immunosuppressants are created equal. Methotrexate, often the first-line treatment, only raises infection risk 1.2 times above normal. It’s not risk-free-liver enzymes can spike, and you need blood tests every few months-but compared to biologics or JAK inhibitors, it’s relatively mild.
Hydroxychloroquine, used for lupus and mild arthritis, is one of the safest options. It barely touches your immune system’s ability to fight infection. Patient reviews on Drugs.com give it a 7.8 out of 10 for safety-far higher than biologics (6.2) or JAK inhibitors (5.9). For people with mild disease, it’s often the best choice.
Calcineurin inhibitors like cyclosporine and tacrolimus are tough on the kidneys. About one in three patients develops kidney damage within two years. And drugs like mycophenolate and azathioprine can suppress bone marrow, leading to low white blood cell counts. That means even a cold can turn into pneumonia if you’re not monitored.
Monitoring Isn’t Optional
The biggest mistake doctors make is treating all immunosuppression the same. You can’t just say, “You’re on a biologic, so watch for infections.” You need to know which part of your immune system is down, and for how long.
The American College of Rheumatology now recommends specific monitoring based on the drug:
- If you’re on Rituximab: get all vaccines at least four weeks before starting. Check antibody levels after vaccination. Test for hepatitis B before and during treatment.
- If you’re on JAK inhibitors: get annual varicella zoster testing. Monitor for signs of blood clots-swelling in legs, chest pain, shortness of breath.
- If you’re on high-dose steroids: get PPD tests twice a year for TB, and monthly blood counts to catch bone marrow suppression early.
A 2022 study found that 72% of serious complications happened because of poor monitoring-not because the drugs were inherently too dangerous. That’s on the system, not the patient.
Vaccines and Timing Matter
Most people don’t realize that vaccines don’t work the same way when you’re immunosuppressed. Live vaccines like MMR or the nasal flu spray are off-limits. Even inactivated vaccines may not stick.
The CDC says you need to be fully vaccinated before starting drugs like Rituximab or other B-cell depleters. After you start, your body won’t respond properly. One study showed 68% of serious infections could have been prevented with timely vaccination.
And here’s the catch: if you’re already on the drug, you can’t just get a vaccine and expect it to work. You might need to wait months after stopping treatment. Some patients end up with no protection against tetanus, measles, or pneumococcus-and they don’t even know it.
Real Stories, Real Consequences
Patients aren’t just numbers. A woman on PatientsLikeMe switched from methotrexate to sulfasalazine because her liver enzymes spiked. Her GI doctor said sulfasalazine was safer long-term, but less effective for her joints. She’s stuck between pain and risk.
Another patient, a 68-year-old smoker with rheumatoid arthritis, started a JAK inhibitor after his TNF blocker stopped working. Six months later, he was diagnosed with lung cancer. His oncologist asked if he’d ever smoked. He said yes. Then the oncologist asked if he’d been on any immunosuppressants. He hadn’t connected the dots.
The Arthritis Foundation’s 2022 survey found that 42% of people stopped biologics because they were scared of infections. Another 28% had been hospitalized for one. These aren’t rare events. They’re predictable-and preventable.
What’s Changing Now
The medical world is waking up. In 2023, the FDA required mandatory training for doctors prescribing JAK inhibitors. Medicare now demands proof of vaccination and infection risk assessment before approving biologics. Insurance companies are catching on.
Researchers are working on ways to predict who’s most at risk. The NIH launched a $28 million project to find biomarkers that show how deeply someone’s immune system is suppressed. Early results suggest analyzing specific T-cell subsets could let doctors tailor monitoring-some patients might need monthly check-ups, others only yearly.
AI tools are being tested too. Mayo Clinic’s prototype used electronic health records to flag patients at high risk of infection. In a pilot, it cut serious infections by 22%. That’s not science fiction-it’s the next step.
The Bottom Line
Immunosuppressants save joints, skin, and organs. But they also leave you vulnerable. The key isn’t avoiding them-it’s understanding them. Know what drug you’re on. Know how it affects your body. Know what tests you need and when. Ask your doctor: Which part of my immune system is being suppressed? For how long? What infections am I most at risk for? What vaccines do I need now?
There’s no one-size-fits-all answer. But if you’re on one of these drugs, you owe it to yourself to be informed-not just compliant.

Josh McEvoy
January 23, 2026 AT 00:43Tiffany Wagner
January 23, 2026 AT 23:20Viola Li
January 24, 2026 AT 14:51Jenna Allison
January 25, 2026 AT 07:59Vatsal Patel
January 26, 2026 AT 06:09Michael Camilleri
January 27, 2026 AT 01:50lorraine england
January 27, 2026 AT 21:06Darren Links
January 29, 2026 AT 02:25Kat Peterson
January 30, 2026 AT 01:32Helen Leite
January 31, 2026 AT 15:23Elizabeth Cannon
January 31, 2026 AT 20:14Karen Conlin
February 1, 2026 AT 18:11asa MNG
February 2, 2026 AT 14:51Heather McCubbin
February 3, 2026 AT 06:21