Aminoglycoside Antibiotics and Kidney Damage: What You Need to Know About Nephrotoxicity
 Nov, 18 2025
Nov, 18 2025
Aminoglycoside Nephrotoxicity Risk Calculator
Patient Risk Factors
Risk Assessment
When you're fighting a serious bacterial infection, especially one caused by tough Gram-negative bugs like E. coli or Pseudomonas, doctors sometimes turn to aminoglycoside antibiotics. Drugs like gentamicin, tobramycin, and amikacin work fast and kill bacteria effectively. But there’s a hidden cost: up to 1 in 4 people on these drugs will develop kidney damage. It’s not rare. It’s not random. And it’s not always caught in time.
How Aminoglycosides Hurt the Kidneys
These antibiotics don’t just float through your body and disappear. About 5% of every dose gets trapped in the cells lining the proximal tubules - the part of your kidney that reabsorbs nutrients and filters waste. Once inside, they pile up in lysosomes, the cell’s recycling centers. That’s where things go wrong. The drugs bind to negatively charged lipids in the cell membrane, disrupting enzyme function. Over time, this leads to swelling of lysosomes, formation of myeloid bodies (fatty waste clumps), and damage to mitochondria and the endoplasmic reticulum. These aren’t just lab observations - they’re what happens inside your kidneys when you’re on aminoglycosides for more than a few days. The result? A slow, silent decline in kidney function. Your serum creatinine rises. Your urine output stays normal (that’s why it’s called nonoliguric), but your kidneys are struggling. You might not feel sick. You might not even notice - until a blood test shows your kidneys aren’t working like they should.Who’s at Risk?
Not everyone gets kidney damage. But some people are far more vulnerable.- If you’re over 65, your risk jumps significantly. Aging kidneys just don’t handle toxins as well.
- If you already have reduced kidney function - say, an eGFR below 60 - your risk triples. That’s not a small increase. It’s a red flag.
- Using other kidney-harming drugs at the same time? That’s a dangerous combo. Vancomycin, for example, raises your risk by nearly three times when paired with gentamicin.
- Dehydration? That’s a big one. Low blood volume means less blood flow to the kidneys, making them more sensitive to the drug’s toxic effects.
- Getting the drug for more than 7 days? The longer you’re on it, the higher the chance of damage.
How Nephrotoxicity Shows Up
This isn’t sudden kidney failure. It creeps in. Most people start showing signs after 5 to 7 days of treatment. The earliest warning signs show up in urine - not blood. You’ll see higher levels of proteins like beta-2-microglobulin, enzymes like N-acetylglucosaminidase, and electrolytes like magnesium and calcium leaking out. These changes happen before creatinine even starts to climb. Clinically, doctors look for a rise in serum creatinine of at least 0.5 mg/dL or a 50% increase from your baseline. That’s the threshold for diagnosing antibiotic-induced kidney injury. And yes - this is still common. A 2021 study of over 1,200 patients found nearly 19% developed acute kidney injury from aminoglycosides.Dosing Matters More Than You Think
Here’s something most patients don’t know: how often you get the dose changes your risk. For years, doctors gave aminoglycosides three times a day. That’s outdated. Research from 2003 showed that giving the same total daily dose in three smaller shots causes faster, deeper kidney damage than giving it all at once. Now, once-daily dosing is the standard. Why? Because your kidneys get a break. The drug clears out between doses, reducing the buildup in tubule cells. But timing matters too. Studies suggest giving the dose around 1:30 p.m. results in less kidney stress than morning or evening doses - likely because of natural daily rhythms in kidney blood flow. And not all aminoglycosides are equal. Gentamicin is the most nephrotoxic. Amikacin is a bit gentler on the kidneys at the same dose. But they all carry the same risk if misused.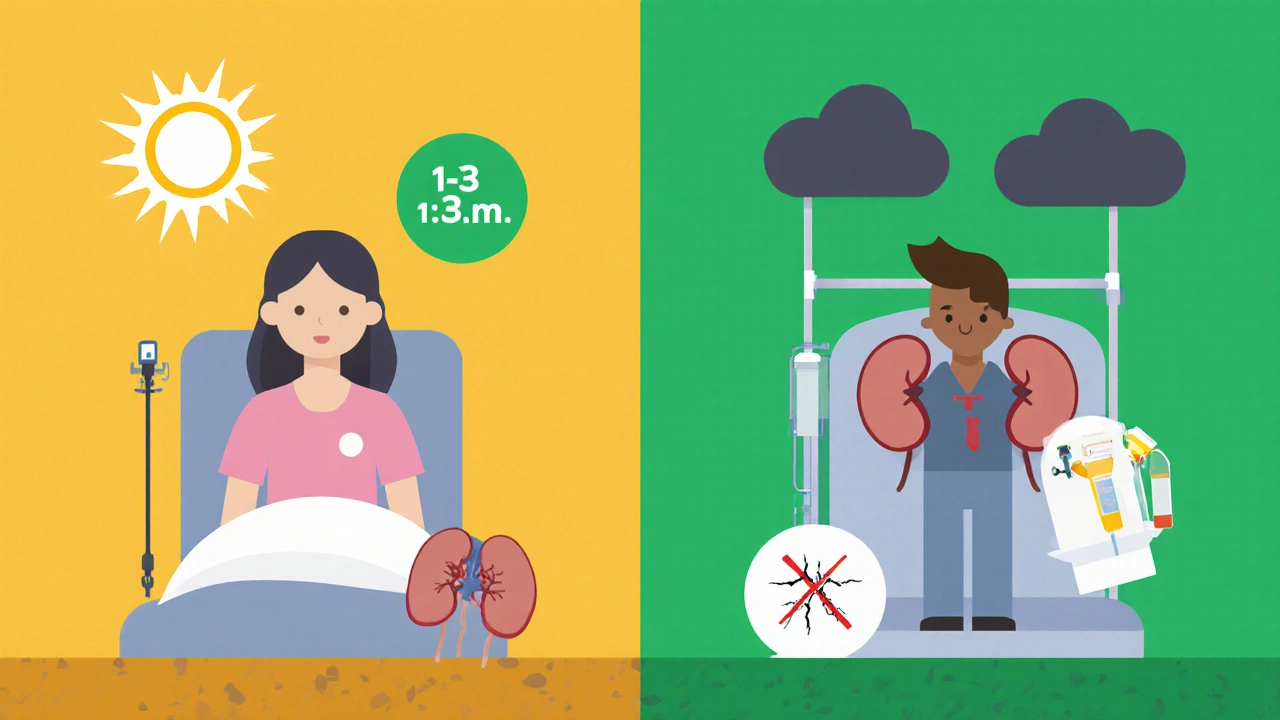
What Doctors Do to Prevent It
Guidelines from the Infectious Diseases Society of America and the European Society of Clinical Microbiology and Infectious Diseases are clear:- Use once-daily dosing - never multiple daily doses unless absolutely necessary.
- Monitor serum creatinine every 48 to 72 hours.
- Keep trough levels (the lowest concentration before the next dose) below 1 μg/mL for gentamicin.
- Avoid combining with other nephrotoxins like vancomycin, NSAIDs, or contrast dye.
- Hydrate. Make sure you’re well-watered before and during treatment.
- Don’t go longer than 7 days unless you have no other option.
Recovery - Is It Possible?
The good news? Most people recover. In the Mayo Clinic study, 82% of patients saw partial or full kidney function return within 30 days of stopping the drug. Recovery usually starts 3 to 5 days after the last dose. Creatinine levels begin to drop. But full recovery can take 1 to 3 weeks. Some people, especially older adults or those with prior kidney issues, never fully bounce back. Permanent loss of kidney function happens in a small but meaningful number of cases. Animal studies show something surprising: with long-term exposure, kidneys can adapt. Rats given high doses of gentamicin for 6 weeks developed severe damage at first - then recovered almost completely. Why? New, less sensitive tubule cells replaced the damaged ones. That’s hope. But it’s not something we can count on in humans.What’s Next? New Hope on the Horizon
Scientists aren’t giving up. They’re looking for ways to block the damage before it starts. One promising candidate is polyaspartic acid. In lab studies, it stops aminoglycosides from sticking to kidney cells. It prevents the buildup of fatty waste, protects mitochondria, and stops cell death. It works in rats, mice, and human cell cultures. But it’s not approved for use in people yet. A modified version of this compound is now in Phase II clinical trials in the U.S. (NCT04567821). If it works, it could be the first real protective drug for aminoglycoside users. Other research is exploring antioxidants that target mitochondrial damage, or drugs that block specific cell death pathways. The National Institutes of Health has invested over $24 million in this area since 2021. That’s a lot of money - and it shows how serious this problem still is.
Why We Still Use Them
You might wonder: if they’re this dangerous, why do we still use them? Because for certain infections - especially those caused by multidrug-resistant bacteria - there are no good alternatives. Aminoglycosides are one of the few drugs that can kill superbugs like carbapenem-resistant Enterobacteriaceae. They’re cheap. They’re effective. And in sepsis or pneumonia in intensive care, they can be life-saving. The World Health Organization estimates 12.5 million treatment courses are given worldwide each year. That’s a lot of people relying on them. The goal isn’t to stop using them. It’s to use them smarter.What You Can Do
If you’re prescribed an aminoglycoside:- Ask: Is this the best option? Are there alternatives?
- Ask: How long will I be on it? Don’t let it go past 7 days without review.
- Ask: Can you check my kidney function before and during treatment?
- Drink water. Don’t wait until you’re thirsty.
- Report any changes - swelling, less urine, fatigue, nausea. Don’t assume it’s just the infection.

Ashley Miller
November 20, 2025 AT 01:09Of course the pharmaceutical giants love aminoglycosides - cheap, patent-free, and perfect for making people dependent on lifelong dialysis. They don’t care if your kidneys turn to dust as long as you keep coming back for the next prescription. And guess who’s funding the ‘research’? Same folks who told us smoking was healthy. Wake up, sheeple.
They’re hiding the polyaspartic acid trials too. Why? Because if you could take a pill to block kidney damage, they’d lose their monopoly on ‘essential’ antibiotics. They need you scared, sick, and paying.
Next thing you know, they’ll patent your urine output and charge you per mL.
Sherri Naslund
November 21, 2025 AT 13:21ok but like… why do we even have kidneys if not to get wrecked by drugs? 🤔
also i think the real problem is that doctors are just lazy and don’t want to learn new stuff. like why not just inject the antibiotic directly into the toilet? that’s where most of it ends up anyway. and why is it always the poor folks who get the toxic ones? coincidence? i think not.
also i read on a forum that aminoglycosides are secretly made from alien DNA and the government uses them to control our dreams. that’s why i keep dreaming about kidney stones shaped like the moon. it’s not a coincidence. it’s a message.
also i think the ‘once daily dosing’ thing is just a marketing ploy to make you think they care. they don’t. they just want you to stop asking questions. and hydration? lol. drink water? like that’s gonna fix a system designed to break you. i drink coffee. and i’m still alive. kinda.
also my cat had a fever last year and i gave her gentamicin from my cabinet. she’s fine. she’s now a spiritual guide. her name is Dr. Squeak. she knows the truth.
Martin Rodrigue
November 21, 2025 AT 16:57While the post presents a clinically accurate overview of aminoglycoside nephrotoxicity, it fails to adequately contextualize the risk-benefit calculus in critical care settings. The 1 in 4 incidence figure is misleading without stratification by duration, therapeutic drug monitoring adherence, and baseline renal function. Moreover, the assertion that ‘kidney damage is not random’ is statistically sound but ontologically reductive - nephrotoxicity remains a multifactorial phenomenon involving genetic polymorphisms in organic cation transporters (OCT2), mitochondrial haplotype variability, and epigenetic modulation of lysosomal biogenesis.
The claim that once-daily dosing reduces tubular accumulation is supported by pharmacokinetic-pharmacodynamic modeling, but the temporal optimization of dosing at 1:30 p.m. lacks robust validation in randomized controlled trials. The cited 2021 study (n=1,200) is retrospective and subject to selection bias. Furthermore, the notion that ‘recovery is possible in 82%’ is misleading without clarification that ‘partial recovery’ often equates to a 15–20% reduction in eGFR - a clinically significant deficit in elderly populations.
Finally, the reference to polyaspartic acid as a ‘promising candidate’ is premature; while in vitro data are encouraging, no Phase III trial has been initiated, and the compound’s bioavailability, renal excretion profile, and potential for off-target effects remain uncharacterized in humans. Until such data are available, adherence to current guidelines remains the gold standard.
rachna jafri
November 21, 2025 AT 22:45They think they can poison us with Western medicine and call it ‘science’? In India, we’ve been healing with turmeric, neem, and yoga for 5,000 years - and still we live longer than your obese, pill-popping Americans. This aminoglycoside nonsense? It’s not medicine - it’s colonial bioweapons disguised as treatment. Why do you think they push these drugs in poor countries? To weaken our bodies before they steal our resources!
My cousin in Delhi got sepsis and took gentamicin for three days. His kidneys? Fine. He drank coconut water, did pranayama, and chanted ‘Om Namah Shivaya’ while lying on the floor. The hospital? They were shocked. He didn’t even need dialysis.
They don’t want you to know that nature heals better than a lab. They want you dependent. They want you afraid. They want you paying for poison. But we - we remember. We are not your test subjects.
And don’t even get me started on the ‘once-daily dosing’ - that’s just a fancy way of saying ‘we’re giving you the same poison, but slower, so you don’t notice until it’s too late.’
darnell hunter
November 22, 2025 AT 00:53The assertion that aminoglycoside nephrotoxicity is preventable through hydration and once-daily dosing is empirically insufficient. The cited 19% incidence rate in the 2021 cohort is consistent with prior meta-analyses, yet the author fails to acknowledge the confounding influence of sepsis-induced acute tubular necrosis, which frequently co-occurs with aminoglycoside administration. The distinction between drug-induced injury and infection-related injury is clinically and statistically nontrivial.
Furthermore, the suggestion that polyaspartic acid represents a viable prophylactic agent is speculative. No peer-reviewed publication in a high-impact journal has demonstrated reproducible efficacy in human renal tubular epithelial cells under physiologic shear stress. The referenced Phase II trial (NCT04567821) has not reported primary outcome data. Until such data are published, the recommendation to ‘watch for trials’ is not evidence-based - it is wishful thinking.
Therapeutic drug monitoring remains the only validated method of risk mitigation. All other interventions - including hydration, timing, and avoidance of concomitant nephrotoxins - are adjunctive and unquantified in their contribution to renal preservation.
It is irresponsible to imply that patient advocacy can supplant clinical vigilance.
Bette Rivas
November 23, 2025 AT 18:45One thing this post doesn’t emphasize enough is how variable the kinetics of aminoglycoside uptake can be between individuals - even with identical dosing. There’s a 2023 paper in Clinical Pharmacology & Therapeutics showing that people with certain SLCO1B1 gene variants clear gentamicin up to 40% slower, which dramatically increases intracellular accumulation in the proximal tubules. That’s not in the guidelines yet, but it should be. Genetic screening isn’t common, but if you’re on this drug for more than 5 days and you’re over 50, it’s worth asking your pharmacist about it.
Also, the ‘nonoliguric’ presentation is a trap. People assume ‘normal urine output’ means ‘fine kidneys,’ but that’s when the damage is most insidious. The tubules are still working enough to make urine, but they’re not reabsorbing anything properly. That’s why you see low magnesium, high urine NAG, and proteinuria before creatinine rises. If your doctor isn’t checking those, they’re not doing their job.
And hydration? Yes, but not just ‘drink water.’ You need isotonic fluids. Plain water dilutes your serum sodium and can actually reduce renal perfusion pressure. IV saline 0.9% before and during therapy is better - if you’re inpatient. Outpatients? Stick to electrolyte drinks with sodium and potassium. Avoid sports drinks with high fructose - they worsen mitochondrial stress.
And yes, amikacin is slightly less toxic than gentamicin - but only by about 15%. The real difference is in resistance patterns. If you’re dealing with a CRE infection, amikacin might be your only shot. But if it’s just a UTI? There are better options. Always ask: ‘Is this the narrowest effective spectrum?’
prasad gali
November 24, 2025 AT 17:14The clinical management paradigm for aminoglycoside-induced nephrotoxicity remains fundamentally reactive rather than predictive. The reliance on serum creatinine as a biomarker is archaic - its lag time exceeds 24–48 hours, rendering it useless for early intervention. The field requires real-time biomarkers: urinary KIM-1, NGAL, and L-FABP are validated in multiple cohorts and should be integrated into standard protocols. Their cost is negligible compared to dialysis.
Furthermore, the concept of ‘once-daily dosing’ is misapplied in many institutions. The pharmacodynamic target is Cmax/MIC > 8–10, not total daily exposure. In patients with fluctuating volume status (e.g., septic shock), peak concentrations may be subtherapeutic, leading to resistance - while troughs remain elevated due to impaired clearance. This creates a double-edged sword: suboptimal efficacy and maximal toxicity.
Therapeutic drug monitoring is not optional. It is the baseline standard of care. Failure to implement it constitutes negligence. The WHO’s global treatment estimates are irrelevant without accountability. If you’re not measuring troughs, you’re not practicing medicine - you’re gambling.
Paige Basford
November 25, 2025 AT 10:11Okay, I just read this whole thing and I’m so glad I asked my doctor about my gentamicin course last month - she actually checked my creatinine every 48 hours and we stopped it at day 6 because my levels were creeping up. I didn’t even know that was a thing you could do!
Also, I was so scared about the kidney thing, but I kept drinking water and eating bananas (for the potassium) and honestly, I felt fine. I think just being aware made a difference. I didn’t just sit there and wait for something to happen.
And that part about the 1:30 p.m. dosing? That’s wild. I didn’t even know time of day mattered. My nurse told me to take it before bed and I was like, ‘Wait, what?’
Anyway, I’m just saying - if you’re on one of these, don’t be shy. Ask questions. Even if they seem dumb. I asked if I could take probiotics and they said ‘probably not during,’ but at least I know now. And hey - I’m alive and my kidneys are still working. Small wins, right?
Ankita Sinha
November 26, 2025 AT 04:08This is the kind of info that should be plastered on every hospital wall. I didn’t know aminoglycosides could cause silent kidney damage - I thought it was just ‘bad side effects’ like nausea. Now I get why my uncle’s creatinine spiked after his pneumonia treatment. He was on it for 10 days and no one checked.
But here’s the thing - if we’re talking about protecting kidneys, why aren’t we talking about diet? I read a study where patients on aminoglycosides who ate more antioxidants (berries, spinach, nuts) had lower oxidative stress markers. It’s not a cure, but it’s a buffer. And hydration? Yes, but not just water - coconut water, cucumber juice, even herbal teas with dandelion root help flush the tubules.
And I love that they’re testing polyaspartic acid. That’s the future. We need more of this - not just ‘don’t do X,’ but ‘do Y to protect yourself.’
Also, if you’re older, have diabetes, or are on diuretics - please, please, please get your eGFR checked before they start this. Don’t wait for symptoms. Your kidneys don’t scream - they whisper. And by the time you hear them, it’s too late.