Adrenal Insufficiency from Corticosteroid Withdrawal: How to Recognize and Manage the Risk
 Nov, 5 2025
Nov, 5 2025
Steroid Withdrawal Risk Calculator
This tool estimates your risk of developing adrenal insufficiency after stopping corticosteroids. Based on current medical guidelines, even short-term use can pose risks.
Your Information
Your Risk Assessment
Based on your steroid use, you have:
Higher risk means more urgent need for medical guidance and emergency medication
Recommended Actions
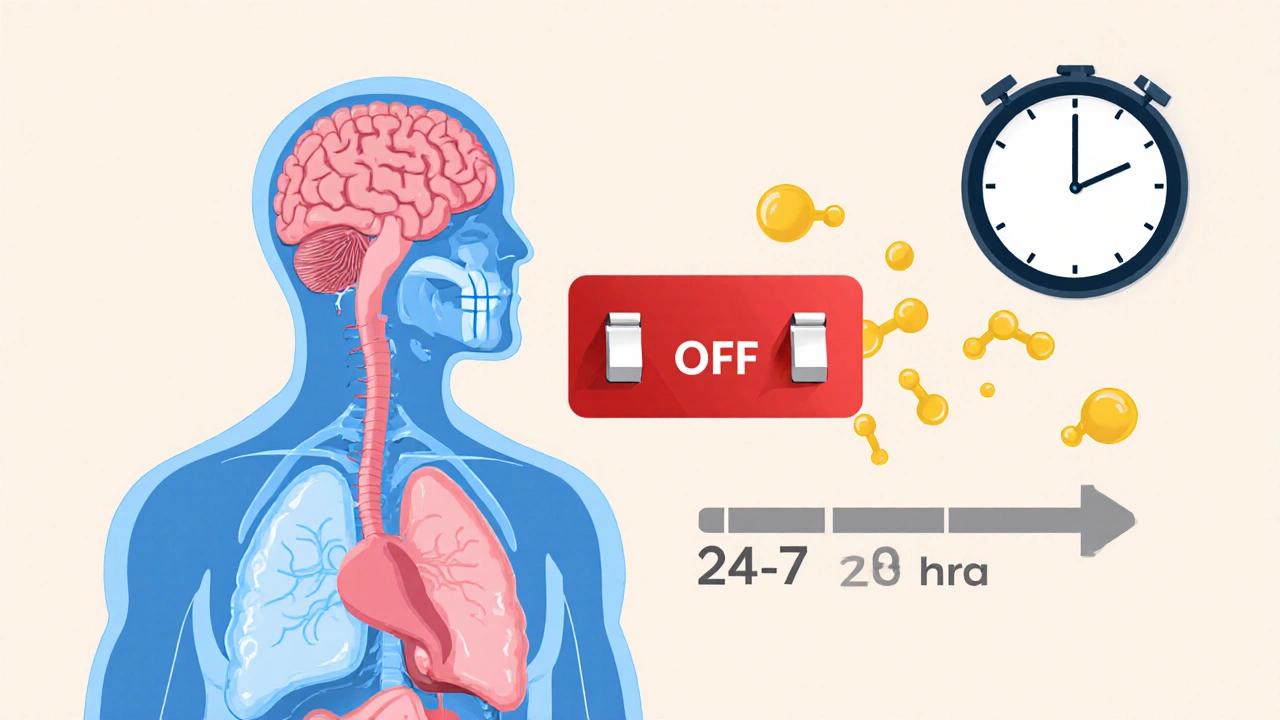
Stopping corticosteroids like prednisone or dexamethasone suddenly can trigger a life-threatening condition called adrenal insufficiency. Many people think if they’ve only taken steroids for a few weeks, they’re safe. That’s not true. Even low doses and short courses can shut down your body’s natural cortisol production. When you stop, your adrenal glands - which normally make cortisol to help you handle stress, regulate blood pressure, and keep your energy up - can’t snap back fast enough. The result? Fatigue so deep it feels like you’re dragging through concrete, nausea, low blood pressure, and sometimes, full-blown adrenal crisis.
Why Your Body Can’t Just Restart
Your body runs on a delicate balance. The hypothalamus tells the pituitary gland to release ACTH, which tells your adrenal glands to make cortisol. When you take external steroids, your brain thinks, “We’ve got plenty,” and shuts off the signal. Over time, your adrenal glands shrink from disuse. It’s like a muscle you stop using - it gets weak. When you stop the pills, your brain doesn’t instantly restart the signal, and your adrenals aren’t strong enough to respond. This isn’t just a side effect - it’s a physiological reset that takes time, and skipping the reset can be deadly.Research shows that even taking as little as 5 mg of prednisone daily for more than four weeks can suppress your natural cortisol production. A 2023 study in Endocrine Abstracts confirmed this, overturning the old belief that only long-term, high-dose use was risky. That means someone on a two-week course for a bad flare-up of asthma or rheumatoid arthritis could still be at risk if they stop cold turkey.
What the Symptoms Look Like - And Why They’re Often Missed
The signs don’t show up right away. They creep in 24 to 72 hours after your last dose. At first, it’s easy to blame something else: “I’m just tired from the flu,” or “My depression is coming back.” But here’s what’s really happening:- Severe fatigue (85% of cases)
- Loss of appetite and unexplained weight loss (72%)
- Nausea, vomiting, or stomach pain (68%)
- Muscle weakness (65%)
- Irritability, anxiety, or low mood (58%)
- Dizziness or fainting when standing up (sign of low blood pressure)
If these symptoms get worse - you start feeling confused, your skin turns pale or blotchy, your heart races, or you pass out - you’re in adrenal crisis. This isn’t a “wait and see” situation. Without emergency treatment, about 6% of hospitalized patients die. A 2024 case report described a 45-year-old woman who thought she had a UTI after stopping dexamethasone. She ended up in the ER with septic shock - until someone checked her cortisol levels. Once she got IV hydrocortisone, she improved in under an hour.
Doctors miss this diagnosis all the time. A 2023 survey of patient forums found that 68% of people had their symptoms dismissed as viral illness, anxiety, or chronic fatigue. One Reddit user wrote: “My doctors kept saying it was post-viral fatigue for six weeks. I ended up in the ER with an adrenal crisis. Now I carry emergency hydrocortisone everywhere.”
Different Types of Adrenal Insufficiency - And Why It Matters
There are three types, and they’re not the same:- Primary: Your adrenal glands are damaged (like in Addison’s disease). You need lifelong replacement.
- Secondary: Your pituitary gland doesn’t make enough ACTH. Often from tumors or surgery.
- Tertiary: Your hypothalamus stopped making CRH - the signal that starts the whole chain. This is what happens with steroid withdrawal.
Tertiary adrenal insufficiency is the most common type caused by medication. It’s temporary - but only if you handle it right. The key difference? In tertiary cases, your cortisol levels will slowly recover over weeks or months if you taper properly. In primary or secondary, recovery usually doesn’t happen without ongoing treatment.
Testing helps confirm it. A morning cortisol level under 5 μg/dL 24 hours after your last dose strongly suggests adrenal insufficiency. Above 10 μg/dL, you’re likely fine. But many clinics don’t test - they assume you’re okay if you tapered “by the book.” That’s risky.

How to Taper Safely - No One-Size-Fits-All
There’s no universal tapering schedule. The Endocrine Society says it depends on how long you’ve been on steroids, the dose, your health, and why you were taking them. But here’s what most experts agree on:- If you’ve taken more than 20 mg of prednisone daily for over 3 weeks - get your adrenal function checked before stopping.
- For doses above 20 mg: Reduce by 2.5-5 mg every 3-7 days.
- For doses between 5-20 mg: Reduce by 1-2.5 mg every 1-2 weeks.
- If you’ve been on steroids longer than 6 months, slow it down even more - sometimes over 3-6 months.
Some people need to pause their taper if they get sick, stressed, or have surgery. Stress - even a dental procedure or a bad cold - can trigger crisis if your body isn’t producing enough cortisol. That’s why patients on long-term steroids are told to “double up” during illness. If you’re tapering, you still need to do this.
A 2023 JAMA study found 47% of patients didn’t follow their tapering plan - often because they were scared of side effects or thought they felt fine. That’s dangerous. Feeling better doesn’t mean your adrenals are back online.
What You Need to Do - Right Now
If you’re on or have recently stopped corticosteroids:- Don’t stop cold turkey. Never reduce or stop without your doctor’s guidance.
- Get written instructions. Ask for a clear tapering plan with exact doses and timelines.
- Carry emergency medication. If you’ve been on steroids for more than 4 weeks, you should have injectable hydrocortisone (like Solu-Cortef) at home. Learn how to use it.
- Wear medical ID. A bracelet or necklace that says “Adrenal Insufficiency - Needs Steroids” can save your life if you’re found unconscious.
- Know the red flags. If you feel worse after stopping - especially with nausea, dizziness, or confusion - go to the ER immediately. Say: “I think I’m having adrenal insufficiency from steroid withdrawal.”
A 2023 Mayo Clinic study found that patients who got a written action plan and injection training were 79% more likely to avoid crisis. That’s not just advice - it’s survival.

What’s Changing in 2025
New tools are coming. In 2024, three point-of-care cortisol tests entered phase 2 trials - they can give results in 15 minutes, right in the doctor’s office. AI algorithms are being trained to predict who’s at highest risk by analyzing EHR data: medication history, lab trends, and comorbidities. One 2024 study showed 92% accuracy in predicting who would develop insufficiency after stopping steroids.Also, the FDA and European Medicines Agency now require all systemic corticosteroid packages to include a patient alert card. Pharmacies in 28 European countries hand them out with every prescription. In the U.S., patient guides are mandatory since 2021 - but many patients never read them.
The big challenge? Corticosteroid use has risen 23% since 2015. More people are on them longer. That means more people are at risk. But with better education, better testing, and better patient tools, the Endocrine Society projects a 30% drop in adrenal crises by 2030.
Final Word: This Isn’t a Minor Risk - It’s a Silent Killer
Adrenal insufficiency from steroid withdrawal isn’t rare. It’s underdiagnosed, misunderstood, and often fatal. You don’t need to be on steroids for years to be at risk. You don’t need to be on a high dose. You just need to stop suddenly.If you’ve taken steroids - even once - and you’re feeling off after stopping, don’t wait. Don’t assume it’s stress or the flu. Check your symptoms. Talk to your doctor. Ask about cortisol testing. Make sure you have emergency medication. Your body didn’t forget how to make cortisol - it just needs time and the right support to remember.
Can adrenal insufficiency happen after just a few weeks of steroids?
Yes. Even short-term use - as little as 4 weeks at doses above 5 mg prednisone daily - can suppress your adrenal glands. Research published in 2023 confirms that adrenal suppression isn’t limited to long-term or high-dose therapy. Stopping suddenly after any prolonged use carries risk.
What should I do if I run out of my steroid medication before my taper is done?
Don’t skip doses. Contact your doctor immediately. If you can’t reach them and you’re feeling unwell - especially with nausea, dizziness, or weakness - take your last prescribed dose and go to the ER. Missing a dose during tapering can trigger adrenal insufficiency. Never wait to feel worse before acting.
Do I need to carry emergency hydrocortisone if I only took steroids for a month?
If you took more than 5 mg prednisone daily for more than 4 weeks, yes. Guidelines from the NIDDK and Endocrine Society recommend emergency injectable hydrocortisone for anyone who’s been on steroids long enough to suppress their adrenal glands. Even if you feel fine, a sudden illness or injury could trigger crisis. Carrying it is like having an EpiPen - it’s a safety net.
Can adrenal insufficiency be permanent after stopping steroids?
In most cases, no. Tertiary adrenal insufficiency from steroid withdrawal is usually temporary. Your adrenal glands can recover - but it takes weeks to months. Recovery depends on how long you were on steroids, your dose, and your body’s ability to restart its own cortisol production. Some people need replacement therapy for 6-12 months. A small percentage may need it longer, especially if they had repeated steroid courses.
How do I know if my symptoms are from adrenal insufficiency or something else?
Look at timing and pattern. If your symptoms started 24-72 hours after stopping steroids and include fatigue, nausea, low blood pressure, and dizziness - especially if they’re getting worse - adrenal insufficiency is likely. Blood tests (morning cortisol and ACTH) can confirm it. If you’ve recently stopped steroids and feel unwell, don’t assume it’s stress, depression, or a virus. Ask for a cortisol test.
Is it safe to stop steroids if I feel great?
Feeling great doesn’t mean your adrenal glands are ready. Steroids suppress your natural system - you can feel fine while your body is still shut down. Stopping too fast can cause crisis days or weeks later. Always follow a doctor-approved tapering schedule, even if you feel fine. Your body’s internal clock doesn’t match how you feel.

Ryan Masuga
November 6, 2025 AT 07:17Man, I never realized how sneaky this stuff is. I was on prednisone for 3 weeks for a bad allergy flare and felt fine after stopping - until I got sick with the flu a week later and nearly passed out in the grocery store. Turned out my body had totally shut down cortisol production. Never thought I’d need to carry an EpiPen-style shot for my own hormones.
William Priest
November 7, 2025 AT 16:47Wow, this post is basically a medical textbook with a pulse. Most people think steroids are like Advil - take it, feel better, toss the rest. But no, your hypothalamic-pituitary-adrenal axis isn’t a light switch, it’s a damn symphony orchestra that needs a conductor’s cue to restart. If you’re not getting cortisol testing before and after tapering, you’re gambling with your life. And yes, 5mg for 4 weeks is enough to wreck your endocrine system. The science is settled.
Jennifer Bedrosian
November 9, 2025 AT 02:52OMG I’m so glad someone finally said this!!! I went through this last year and my doctors kept telling me I was just ‘anxious’ or ‘burnt out’ - like I was making it up?? I ended up in the ER with my blood pressure at 78/45 and they didn’t even think to check cortisol until my mom screamed at them. Now I carry my hydrocortisone in my purse like my wallet. If you’re on steroids, PLEASE don’t be like me and wait until you’re almost dead to speak up. You’re not crazy - your adrenals are just on vacation.
Lashonda Rene
November 10, 2025 AT 22:03I’ve been on and off steroids for years because of my autoimmune thing and I didn’t know any of this until I almost died after stopping cold turkey. I thought if I felt okay then I was fine but nope my body was just holding its breath. It took months to feel normal again and I wish I had known about the emergency shot earlier. Now I tell everyone I know who’s on prednisone to ask their doctor for a taper plan and a prescription for Solu-Cortef. It’s not scary if you’re prepared. It’s scary if you’re not.
Rashmi Mohapatra
November 12, 2025 AT 20:08People need to stop being lazy with meds. If you’re gonna take steroids then you gotta follow the rules. You think your body owes you a quick fix? Nah. You messed with your hormones now you pay the price. I’ve seen too many Americans think they’re too busy to taper. Newsflash: your life isn’t more important than your biology.
Abigail Chrisma
November 14, 2025 AT 04:50Thank you for writing this with such clarity. I’m from a community where people avoid doctors unless they’re dying - and steroid use is super common for asthma and eczema. I’m sharing this with my mom, my cousin, my auntie - everyone. I didn’t know about tertiary adrenal insufficiency until now. I’m going to get my medical ID bracelet this week. If this saves one person from an ER trip, it’s worth it.
Ankit Yadav
November 15, 2025 AT 00:06Just had a patient come in last week who thought they were fine after stopping dexamethasone for a week. Got sick, collapsed at work. Cortisol was 2.1. They were lucky. The real issue? Doctors don’t educate patients. We’re taught to taper but not why. This post nails it. We need mandatory patient handouts in every pharmacy. Not just legal checkboxes - real education.
Andy Slack
November 15, 2025 AT 12:31Just got my emergency kit in the mail today. Took me 6 months to finally do it after reading this. I’m not scared anymore. I’m prepared. If you’re on steroids - do this. It’s not overkill. It’s insurance for your life. You don’t wait for a fire to buy a smoke detector. Don’t wait for a crisis to get your shot.